Health is a crown on the heads of the healthy that only the sick can see.

🔥🧬 Evaluation Methods for Brown Adipose Tissue (BAT)
Discover the most effective methods for evaluating Brown Adipose Tissue (BAT), including PET-CT scans, infrared thermography, and biochemical markers. Learn how BAT assessment supports metabolic health, obesity treatment, and fasting research.
MUSCULOSKELETAL
DR Hassan Alwarraqi
1/10/2025
🔥🧬 Evaluation Methods for Brown Adipose Tissue (BAT)
Discover the most effective methods for evaluating Brown Adipose Tissue (BAT), including PET-CT scans, infrared thermography, and biochemical markers. Learn how BAT assessment supports metabolic health, obesity treatment, and fasting research.
Comprehensive Guide to Methods for Evaluating Brown Adipose Tissue (BAT)
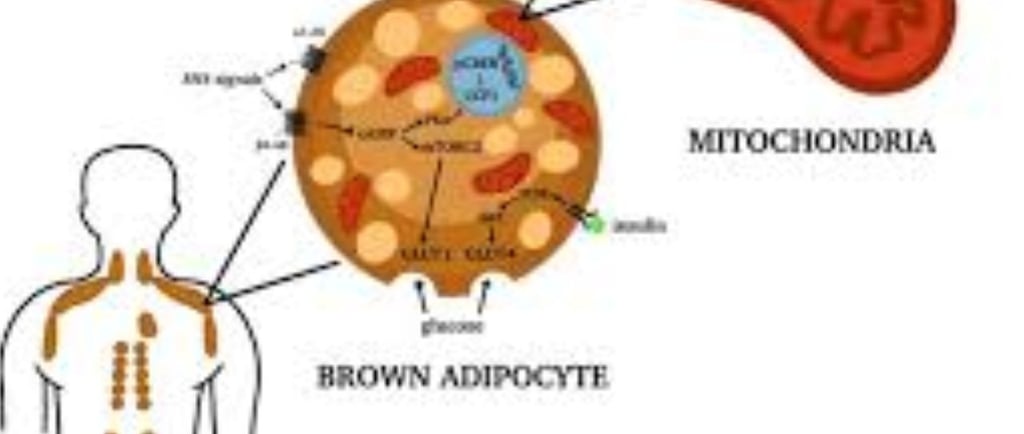
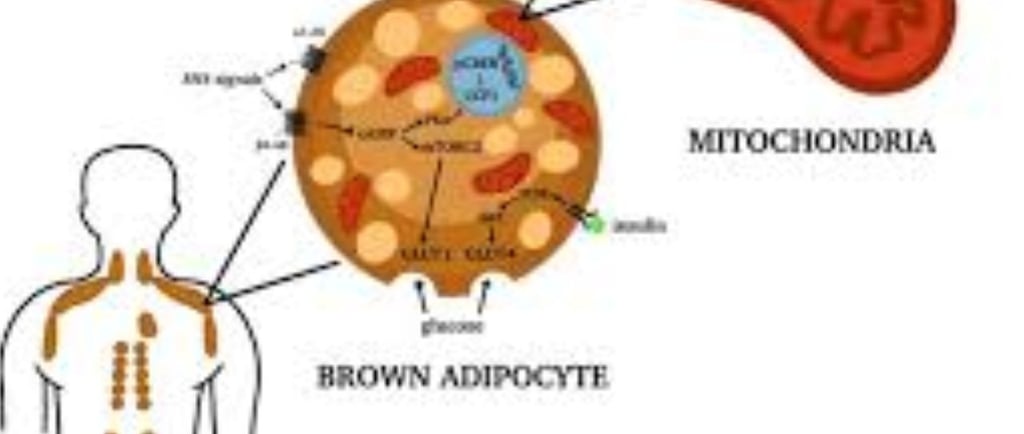
Understanding Brown Adipose Tissue (BAT) and Its Clinical Significance
Brown adipose tissue (BAT) represents a specialized form of fat that plays a crucial role in thermogenesis - the process of heat production through energy expenditure.
Unlike white adipose tissue (WAT) that primarily stores energy, BAT burns calories to generate heat, making it a promising therapeutic target for obesity and metabolic disorders
Recent research has revealed that BAT:
Contains multilocular lipid droplets and abundant mitochondria
Expresses uncoupling protein 1 (UCP1) which enables thermogenesis
Shows higher vascularization and innervation compared to WAT
Can be activated by cold exposure or pharmacological stimulation
The rediscovery of metabolically active BAT in adult humans has sparked significant interest in its potential for treating metabolic diseases.
However, accurate assessment of BAT volume and activity remains challenging, driving the development of various imaging and evaluation techniques
Gold Standard: PET/CT with 18F-FDG
Positron Emission Tomography/Computed Tomography (PET/CT) using 2-deoxy-2-[¹⁸F]fluorodeoxyglucose (18F-FDG) remains the most established method for BAT detection and quantification
How it works:
18F-FDG is taken up by glucose transporters in metabolically active cells
The radioactive tracer accumulates in activated BAT
PET detects gamma rays from positron emission
CT provides anatomical localization
Advantages:
High sensitivity for detecting activated BAT
Provides both metabolic and anatomical information
Established quantification protocols (SUV measurements)
Widely available in clinical settings
Key limitations:
Exposure to ionizing radiation (5-10 mCi per scan)
Only detects activated BAT (misses quiescent tissue)
Glucose uptake may not directly correlate with thermogenesis
Expensive (high equipment and tracer costs)
Requires cold activation protocols for optimal detection
Recent studies suggest BAT glucose uptake primarily supports de novo lipogenesis rather than directly reflecting thermogenic activity, potentially limiting the physiological interpretation of 18F-FDG PET results
Alternative PET Tracers for BAT Imaging
Researchers have explored several alternative PET tracers to overcome 18F-FDG limitations:
Fatty acid tracers (e.g., ¹⁸F-FTHA):
Better match BAT's preferred metabolic substrate
Limited by competition with endogenous fatty acids
¹¹C-Acetate:
Measures oxidative metabolism and blood flow
Requires on-site cyclotron due to short half-life
¹⁵O-labeled compounds:
Directly assess oxygen consumption
Extremely short half-life limits practicality
Neurotransmitter analogs (e.g., ¹⁸F-Dopamine, ¹¹C-MRB):
Target sympathetic innervation of BAT
Provide information about regulatory pathways While these alternatives show promise, none have yet surpassed 18F-FDG in clinical utility for BAT assessment
Magnetic Resonance Imaging (MRI) Approaches
MRI offers several radiation-free alternatives for BAT evaluation:
1. Structural MRI Techniques
T1/T2-weighted imaging: Distinguishes BAT from WAT based on relaxation times
Dixon-based methods: Quantifies fat-water fractions (FWF)
Diffusion-weighted imaging: Assesses tissue microstructure
2. Functional MRI Methods
Blood Oxygen Level Dependent (BOLD) MRI: Measures oxygenation changes during activation
MR Thermometry: Detects temperature changes in BAT
MR Angiography: Visualizes BAT vascular network
3. Advanced Metabolic MRI
Chemical Exchange Saturation Transfer (CEST): Particularly creatine CEST (Cr-CEST) shows promise for detecting BAT activation through creatine metabolism
Hyperpolarized ¹³C MRI: Tracks real-time metabolism but requires specialized equipment
Multinuclear MRS: Using ³¹P, ²H, or ¹³C to study BAT biochemistry
A recent breakthrough in Cr-CEST MRI has demonstrated the ability to:
Detect BAT activation in both rodents and humans at 3T
Correlate with 18F-FDG PET findings
Show changes in creatine concentration during activation
Provide simultaneous fat content and metabolic function imaging
Advantages of MRI:
No ionizing radiation
Excellent soft tissue contrast
Multiple contrast mechanisms
Suitable for longitudinal studies
Challenges:
Longer scan times
Higher equipment costs
Need for specialized sequences
Sensitivity to motion artifacts
Computed Tomography (CT) Methods
CT provides anatomical information about BAT depots:
Single-energy CT:
Identifies BAT based on Hounsfield units (-100 to -30 HU)
Limited specificity due to overlap with WAT values
Dual-energy CT (DECT):
Improves differentiation using dual-energy measurements
Can assess tissue hydration differences
Still involves significant radiation exposure
CT alone cannot assess metabolic activity and is primarily used in combination with PET .
Other Emerging Imaging Modalities
1. Contrast-Enhanced Ultrasound (CEUS)
Measures BAT perfusion changes during activation
Low-cost and portable
Limited by operator dependence and tissue depth
2. Near-Infrared Spectroscopy (NIRS)
Assesses tissue oxygenation and hemodynamics
Completely non-invasive
Limited penetration depth (2-5 cm)
3. Optoacoustic Imaging (MSOT)
Combines optical and ultrasound principles
Label-free detection of hemoglobin changes
Cross-sectional imaging limits volumetric assessment
4. Infrared Thermography
Measures skin temperature over BAT depots
Completely non-invasive and low-cost
Only assesses superficial BAT
Biochemical and Molecular Assessment Methods
While imaging dominates BAT evaluation, complementary techniques include:
Biopsy and Histology:
Gold standard for UCP1 confirmation
Invasive and limited to accessible depots
Microdialysis:
Measures extracellular metabolites
Provides real-time metabolic information
Technically challenging
Gene Expression Profiling:
Quantifies thermogenic markers (UCP1, PGC1α)
Requires tissue samples
Current Challenges in BAT Assessment
Despite technological advances, several key challenges remain:
Differentiation from Beige/Brite Fat:
Current methods cannot reliably distinguish classical BAT from induced beige adipocytes
Quantification Standards:
Lack of consensus on BAT volume measurements
Variable thresholds for activity detection
Physiological Interpretation:
Relating imaging signals to actual thermogenic capacity
Understanding discordance between glucose uptake and thermogenesis
Technical Limitations:
Depth penetration for optical methods
Spatial resolution for small depots
Scan duration for dynamic studies
Future Directions in BAT Evaluation
The field is moving toward:
Multimodal Imaging Approaches:
Combining PET/MRI for comprehensive assessment
Integrating functional and metabolic information
Novel Metabolic Probes:
Developing BAT-specific MRI contrast agents
Exploring hyperpolarized substrates
Standardization Efforts:
Establishing consensus protocols
Developing reference databases
Artificial Intelligence Applications:
Automated BAT detection and segmentation
Prediction of metabolic activity from imaging features
Non-imaging Biomarkers:
Identifying circulating markers of BAT activity
Developing breath tests for thermogenesis
Clinical and Research Applications
Accurate BAT assessment methods enable:
Obesity and Metabolic Disease Research:
Understanding BAT's role in energy balance
Evaluating therapeutic interventions
Drug Development:
Screening BAT-activating compounds
Monitoring treatment responses
Personalized Medicine:
Identifying high BAT responders
Tailoring metabolic therapies
Physiological Studies:
Investigating cold adaptation
Understanding seasonal variations
Conclusion: Toward Optimal BAT Evaluation
The ideal BAT assessment method would combine:
No ionizing radiation
Detection of both active and quiescent BAT
High spatial resolution and specificity
Quantitative metabolic information
Cost-effectiveness and clinical practicality
While current methods each have strengths and limitations, the rapid development of imaging technologies—particularly advanced MRI techniques like Cr-CEST—promises to overcome many existing challenges 4. As our understanding of BAT biology grows, so too will our ability to accurately measure its mass and activity, opening new avenues for combating obesity and metabolic disorders through targeted BAT activation.
Continued innovation in BAT assessment methodologies will be crucial for translating basic research findings into clinical applications and realizing the therapeutic potential of this remarkable thermogenic tissue
What is Brown Adipose Tissue (BAT) and why is it important?
Brown adipose tissue (BAT) is a type of fat tissue recently discovered in the human body, showing promising potential as a therapeutic target for combating obesity and associated metabolic disorders.
BAT differs from traditional white adipose tissue (WAT) due to its ability to burn calories to produce heat, a process known as thermogenesis.
This makes BAT important in energy regulation and may play a role in fighting obesity and metabolic diseases.
What is the most commonly used method for evaluating Brown Adipose Tissue (BAT) today?
The most commonly used and reliable technique for detecting and quantifying active brown adipose tissue in humans is Positron Emission Tomography/Computed Tomography (PET/CT) using
2-deoxy-2-[18F]fluorodeoxyglucose (18F-FDG). This technique involves injecting a radioactive tracer (18F-FDG), which is absorbed by metabolically active cells, and then imaging it using a PET/CT scanner.
However, this method exposes the patient to radiation and can only detect active brown adipose tissue (e.g., after cold exposure) and not inactive BAT.
What are the main limitations of the PET/CT method for evaluating Brown Adipose Tissue (BAT)?
In addition to radiation exposure, one of the main limitations of PET/CT is that it can only detect active brown adipose tissue, failing to identify inactive BAT.
This means the method may not accurately reflect the total amount of brown adipose tissue in the body. Furthermore, PET/CT is costly and requires specialized equipment.
What are the alternative methods available for evaluating Brown Adipose Tissue (BAT)?
Several alternative methods have been developed to overcome some limitations of PET/CT, including:
Magnetic Resonance Imaging (MRI): MRI can be used to assess the volume and fat content of brown adipose tissue, as well as changes in blood flow.
Positron Emission Tomography (PET) with other tracers: Other more specific tracers for brown adipose tissue can be used.
Computed Tomography (CT): CT can evaluate the size of brown adipose tissue, but its ability to assess metabolic activity is limited.
Contrast-enhanced Ultrasound: This technique is used to evaluate blood flow in brown adipose tissue.
Near-infrared Spectroscopy: A non-invasive technique used to assess oxygen levels in tissues.
Temperature measurement of brown adipose tissue areas: Temperature can be measured in areas containing BAT.
PET/MRI Imaging: Combines the advantages of both PET and MRI for a comprehensive assessment of brown adipose tissue.
Single Photon Emission Computed Tomography (SPECT): Another imaging method using radioactive materials to visualize tissue activity.
What are the advantages and disadvantages of these alternative methods?
Each alternative method has its pros and cons.
For example, MRI is safe and does not involve radiation, but it is expensive and may not be available at all centers.
PET/MRI offers comprehensive information but is also costly and complex.
Ongoing research aims to develop more accurate, effective, and cost-efficient methods for evaluating brown adipose tissue.
Are current methods for evaluating Brown Adipose Tissue (BAT) ideal?
No, current methods for evaluating brown adipose tissue are still under development and improvement.
Although PET/CT is the most widely used technique, it has limitations, necessitating further research to develop more effective, accurate, and cost-efficient methods with minimal or no radiation exposure.
What is the goal of developing new methods for evaluating Brown Adipose Tissue (BAT)?
The goal of developing new methods for evaluating brown adipose tissue is to create precise, non-invasive, reproducible, and practical tools to assess the quantity and metabolic function of brown adipose tissue in umans.
These tools will help researchers better understand BAT's physiological role in metabolic regulation and contribute to the development of new treatments for obesity and other metabolic diseases.
What are the future steps in Brown Adipose Tissue (BAT) evaluation research?
Future steps in BAT evaluation research include:
Improving current methods like MRI and PET with other tracers beyond 18F-FDG.
Applying methods tested in preclinical models to humans.
Developing new techniques for evaluating brown adipose tissue, including advanced imaging and metabolic analysis.
Focusing on developing non-invasive, cost-effective, and reproducible methods.
Validating these new methods through clinical studies.
These efforts will lead to a better understanding of brown adipose tissue's role in metabolic regulation and open new avenues for developing effective treatments to combat obesity and metabolic diseases.
KEYWORDS
Brown Adipose Tissue, BAT, metabolic disorders, obesity, thermogenesis, PET/CT, 18F-FDG, MRI, alternative methods, non-invasive evaluation, metabolic function, metabolic regulation, imaging techniques, SPECT, PET/MRI, clinical studies, fat tissue, energy regulation.
🔥🧬 Evaluation Methods for Brown Adipose Tissue (BAT)
✍️ About the Author
Hassan Al-Warraqi is the founder of H-K-E-M.com, and a dedicated researcher in the fields of metabolic health, fasting, and natural therapies. He focuses on uncovering how the body’s innate systems—like brown adipose tissue (BAT)—can be activated for healing and weight regulation.
In this article, Hassan outlines the most advanced and emerging methods for evaluating BAT, including PET-CT scans, infrared thermography, and biochemical markers, highlighting their role in understanding metabolism and potential treatments for obesity, diabetes, and chronic fatigue.
📱 Short Social Media Version
🖋️ By Hassan Al-Warraqi
Founder @h_k_e_m_com | Curious about brown fat? 🔥 Discover how science measures BAT for metabolic health! 🧬 #BrownFat #Metabolism #HKEM