Health is a crown on the heads of the healthy that only the sick can see.
🏠💨🫁 Home Oxygen Therapy & The Only Hope 🌟🙏
🏠💨🫁 Home Oxygen Therapy & The Only Hope 🌟🙏 – Discover how home oxygen therapy can improve breathing, boost quality of life, and offer renewed hope for patients with chronic respiratory conditions, along with safe usage tips and expert guidance.
RESPIRATORY SYSTEM
Dr Hassan Al Warraqi
8/15/20259 min read


🏠💨🫁 Home Oxygen Therapy & The Only Hope 🌟🙏
🏠💨🫁 Home Oxygen Therapy & The Only Hope 🌟🙏 – Discover how home oxygen therapy can improve breathing, boost quality of life, and offer renewed hope for patients with chronic respiratory conditions, along with safe usage tips and expert guidance.
Essential Insights for Lung Health
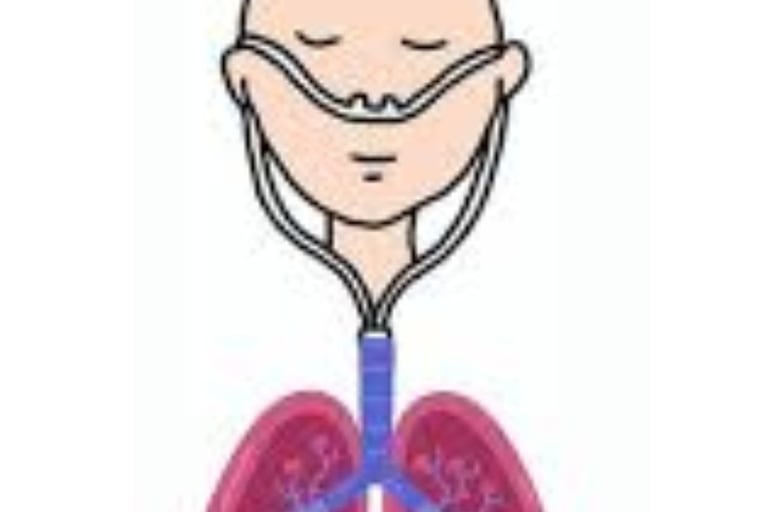
Understanding Home Oxygen Therapy
Home oxygen therapy is a critical medical intervention prescribed for individuals with chronic conditions like COPD, pulmonary
fibrosis, and heart failure that result in low blood oxygen levels.
This treatment ensures adequate oxygenation, helping to prevent serious complications associated with hypoxemia.
How Oxygen Therapy Improves Quality of Life for Lung Conditions
For those battling conditions such as COPD and pulmonary fibrosis, oxygen therapy offers significant relief by reducing
breathlessness and boosting overall quality of life.
Though adapting to home oxygen might feel daunting at first, it empowers patients to sustain their activity levels and continue
enjoying daily routines and hobbies.
Building a support system is vital—patients benefit greatly from discussing their therapy with family and friends to gain
understanding and maintain a sense of normalcy.
Key Safety Guidelines for Using Home Oxygen Equipment
While oxygen itself isn't flammable, it dramatically accelerates combustion, making fire safety a top priority for users.
No Smoking Policy: Absolutely no smoking or open flames are permitted near oxygen equipment. Post clear "No Smoking"
and "No Open Flames" signs as reminders.
Heat Source Clearance: Maintain at least a five-foot distance from all heat sources and open flames.
Electrical Appliance Caution: Avoid using devices like hair dryers, curling irons, electric razors, or gas stoves while on
oxygen.
Flammable Product Avoidance: Do not use aerosol sprays (e.g., air fresheners, hairspray) or oil-based products (e.g.,
petroleum jelly) near oxygen; opt for water-based alternatives.
Equipment Care: Never oil the oxygen unit and handle it with clean, non-greasy hands. Ensure concentrators are positioned
away from walls and curtains for ventilation and never cover them.
Tubing Safety: Watch for tripping hazards with tubing, and never cut it or use lengths over 50 feet.
Power Outage Preparedness: Have a contingency plan for outages, including access to portable tanks, notifying your power
company of life-sustaining equipment needs, and considering a backup generator.
Supply Management: Regularly check gauges and order refills in advance.
Hygiene Maintenance: Clean humidifier bottles weekly with soap and water to prevent bacterial growth. Replace nasal
cannulas frequently and main tubing every 1-2 months, keeping extras on hand.
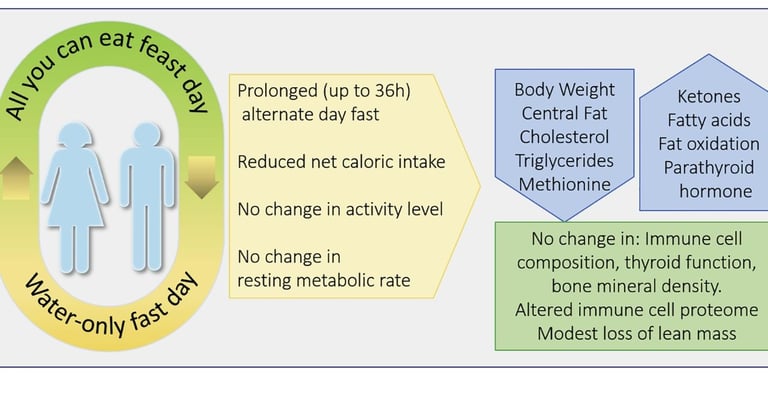
Physiological Effects of Voluntary Fasting
Voluntary fasting, encompassing intermittent and water-only fasting, induces several physiological changes that may impact
health:
Anti-Inflammatory Benefits: Fasting can decrease systemic inflammation and oxidative stress.
Cardiovascular and Metabolic Improvements: Pilot studies show supervised water-only fasting can lower blood pressure
and enhance metabolic parameters in hypertensive patients.
Cellular Metabolism Shifts: It increases ketone body production, potentially triggering adaptive, protective cellular
responses.
Vascular Reactivity Impact: Short-term fasting and dehydration may reduce retinal vascular reactivity due to changes in
nitric oxide and other vasoactive substances, as suggested by case reports, which caution about potential confounding
effects in clinical assessments.
Interactions Between Oxygen Therapy and Fasting
Emerging research indicates that hypoxia (low oxygen levels, whether environmental or controlled) might influence hunger
hormones, brain blood flow, neuroplasticity, and metabolic regulation.
However, there are no well-documented interactions or contraindications specifically between home oxygen therapy and
voluntary fasting in clinical settings. Standard medical advice emphasizes that fasting must be supervised and customized to
the individual’s health status, particularly for those on oxygen therapy.
Fasting can disrupt hydration and electrolyte balance, a significant concern for home oxygen patients with chronic illnesses.
Dehydration and metabolic stress could exacerbate underlying cardiopulmonary conditions, necessitating caution.
Fasting During Ramadan and Oxygen Uptake
Studies suggest that Ramadan fasting does not impair maximum oxygen uptake in healthy adults.
However, special populations, including those reliant on home oxygen, require personalized medical evaluations to ensure
safety.
Practical Considerations for Fasting with Lung Conditions
For patients using home oxygen who wish to fast, rigorous medical oversight is non-negotiable.
Close monitoring of hydration, electrolytes, and overall clinical status is essential, as acute metabolic stress or dehydration can
worsen cardiopulmonary issues.
Medical Consultation: Fasting is typically designed for healthy individuals. If you have a lung condition like asthma, COPD,
pulmonary fibrosis, or cystic fibrosis, consult your doctor or specialist beforehand to assess safety and treatment impacts.
Well-managed conditions might allow fasting under guidance.
Medication Timing: Work with your healthcare provider to adjust medication schedules (e.g., timing preventer inhalers
between Iftar and Suhoor). Inhaled medicines, nebulizers, nasal sprays (if not swallowed), home oxygen therapy, and
injections typically do not break a fast, unlike most oral medications.
Hydration Focus: Dehydration thickens mucus, hindering lung clearance and potentially worsening symptoms. Prioritize
water-rich foods and ample fluids during non-fasting windows.
Dietary Choices: Opt for easily digestible, healthy foods like soups, fruits, and yogurt when breaking fast. Avoid high-salt
and high-sugar items that promote dehydration. Choose starchy, high-fiber, or wholegrain foods at Suhoor for sustained
energy.
Physical Activity: Limit to gentle or moderate exercise like walking, stretching, or yoga, ideally in cool environments.
Health Monitoring: If feeling unwell, stop fasting immediately, follow your prescribed action plan, and seek medical help if
symptoms persist.
Fasting Alternatives: If unable to fast, consider making up days later or fulfilling spiritual obligations through acts of charity.
Therapeutic Potential of Intermittent Hypoxia Training
Intermittent hypoxia training, involving controlled cycles of low-oxygen exposure, offers potential health benefits when carefully
managed:
Hormonal Regulation: Reduces stress hormones (cortisol) and hunger hormones (ghrelin), while boosting hormones linked
to pleasure (dopamine), relaxation (GABA, melatonin), socialization (oxytocin), happiness (beta-endorphins), bliss
(anandamide), and mood stability (serotonin).
Brain Health: Enhances brain blood flow by up to 20%, supports neurogenesis (new nerve cell growth), improves synaptic
plasticity, offers neuroprotection, and may enhance executive functions, attention, and memory.
Metabolic & Anti-Inflammatory Benefits: Improves glucose metabolism and insulin sensitivity, lowers oxidative stress and
inflammation markers (e.g., C-reactive protein), and boosts antioxidants.
Mood and Consciousness: Eases anxiety, improves mood by reducing tension and depression, and can induce altered
states like euphoria or spiritual experiences, potentially increasing pain tolerance.
Methods to Achieve Therapeutic Hypoxia
Breath Control Training: Techniques such as breath-holding (e.g., Kumbhaka pranayama) or prolonged expiration.
Blood Flow Restriction (BFR): Using a tourniquet or cuff on a limb during exercise to create localized hypoxia.
Chanting: Rhythmic vocalization that may lead to oxygen deprivation and altered consciousness.
Hypoxic Gas Mixtures: Inhaling low-oxygen air via masks or chambers.
Rebreathing: Methods like breathing into a paper bag to manage anxiety by reducing oxygen levels.
Digital Support for Low-Oxygen Training
Monitoring Devices: Pulse oximeters and wearable apps track oxygenation in real-time with alerts.
Breathing Apps: Offer guided hypoxic exercises (e.g., "Hypoxic - Breathing Exercises" app) to improve adaptability, reduce
stress, and enhance focus, often with heart rate variability (HRV) analysis.
Visualization & Gamification: Apps with visual aids (e.g., expanding circles) and gamified features (badges, leaderboards)
increase engagement.
Virtual Reality (VR): Combines biofeedback for respiration control in immersive settings, using avatars for enhanced
involvement.
Telehealth: Enables remote training with monitored sessions via wireless sensors.
Specialized Equipment: Devices like hypoxicators facilitate controlled intermittent hypoxia.
These technologies foster breathing metacognition—awareness and adaptation of patterns—supporting physical, cognitive,
and emotional growth.
Challenges in Managing Home Oxygen Therapy
Equipment and Daily Life Challenges
Equipment Bulk: Oxygen concentrators are often large, noisy, and heat-generating, making living spaces uncomfortable.
Mobile tanks, while quieter, are heavy and cumbersome to transport.
Cannula Management for Infants: Keeping nasal cannulas on active babies is tricky; strategies include running tubing up the
back of shirts or applying during sleep.
Tubing Hazards: Long tubing poses tripping risks or can snag on furniture. Securing initial sections to the floor with cord
ties helps mitigate this.
Daily Impact: Navigating errands and outings with tanks and monitors is complex, yet many families adapt to maintain nearnormal
routines.
Monitoring and Health Management
Alarm Fatigue: Pulse oximetry monitors often trigger false alarms due to movement or sensor issues, causing stress; some
parents seek more reliable probes.
Weaning Delays: Frequent medical assessments for weaning off oxygen are ideal, but home settings often require waiting
for formal sleep studies, delaying progress.
Support Systems: Initial home nursing visits, support groups like "Oxygen Users" forums or "Better Breathers Clubs," and
resources such as the American Lung Association's Lung HelpLine offer critical advice and emotional backing.
Home Oxygen Therapy and Fasting: Safety and Supervision
Physiological Interactions
Metabolic Dynamics: Fasting typically lowers metabolic rate, potentially reducing oxygen demand, but it also induces
complex changes in heart rate, blood pressure, and cellular metabolism that could affect oxygen delivery.
Hydration and Electrolyte Risks: Fasting can disrupt fluid and electrolyte balance, a particular concern for those on home
oxygen, as dehydration may thicken blood and strain the heart, increasing oxygen needs.
Critical Need for Medical Oversight
Mandatory Supervision: Patients on home oxygen considering fasting must have close medical oversight. Monitoring
hydration, electrolytes, and clinical status is vital to prevent worsening of cardiopulmonary conditions.
Personalized Assessment: Suitability for fasting varies with individual health status, disease severity, and medication needs.
Shorter, gentler fasting periods (e.g., 12-16 hours) might be more feasible for some, but only under guidance.
Team Approach: Working with a healthcare team ensures fasting plans support respiratory health without compromising
wellbeing.
Conclusion: Balancing Benefits and Risks أف
While voluntary fasting may offer benefits like reduced inflammation and improved metabolism, its safety for individuals on
home oxygen therapy hinges on rigorous clinical assessment.
Risks such as dehydration, metabolic disturbances, and symptom overlap with hypoxemia necessitate caution.
Until more definitive research emerges, the safest path for many may be to leverage religious exemptions for health reasons,
prioritizing medical stability over fasting under strict, individualized supervision.
FAQ: Oxygen Therapy, Lung Health, and Fasting
1. How does oxygen therapy enhance quality of life for those with lung conditions?
Answer:
Reduces Breathlessness: Oxygen therapy helps alleviate shortness of breath in conditions like COPD and pulmonary
fibrosis.
Maintains Activity Levels: Many patients can continue hobbies and daily routines even while on oxygen.
Facilitates Normalcy: Discussing therapy with family/friends in advance helps build a support network, making the
transition smoother.
2. What are the essential safety guidelines for using home oxygen equipment?
Answer:
No Smoking Policy: Keep all smoking and open flames away from oxygen. Clearly post "No Smoking" and "No Open
Flames" signs.
Heat Source Clearance: Maintain at least a five-foot distance from heaters, stoves, and open flames; avoid appliances like
hair dryers and curling irons while on oxygen.
Avoid Flammable Products: Use water-based rather than aerosol or oil-based products near oxygen.
Equipment Care: Never oil the oxygen unit; keep it clean, dry, and away from walls or curtains. Never cover the
concentrator.
Tubing Safety: Watch for tripping hazards and never cut tubing or use lengths beyond 50 feet.
Power Outages: Have backups such as portable tanks and a generator, and inform your utility provider about lifesustaining
equipment.
Refills and Cleaning: Monitor gauges, clean humidifier bottles weekly, and reorder supplies in advance.
Cannulas/Tubing Replacement: Replace frequently (main tubing every 1-2 months).
•3. Which considerations apply to individuals with lung conditions who wish to fast (e.g., during Ramadan)?
Answer:
Consult a Specialist: If you have asthma, COPD, pulmonary fibrosis, or cystic fibrosis, ask your doctor if fasting is safe
given your treatment.
Medication Timing: Coordinate with your healthcare provider about medication schedules (e.g., inhalers, nebulizers).
Remember that oxygen therapy and most injections do not break a fast.
Hydration: Fasting can worsen mucus thickness; drink extra fluids when not fasting to prevent dehydration.
Balanced Diet: Break fast with nutritious foods like soups, fruits, yogurt; avoid salty or sugary items.
Activity & Unwell Feelings: Light exercise in cool environments is advised; stop fasting if you feel worse and seek medical
help.
Exemptions: The Qur’an exempts the physically ill from fasting if it compromises health. Alternative spiritual acts or making
up fasts later can fulfill religious obligations.
4. How does Ramadan fasting affect inflammatory and blood markers in stable COPD patients?
Answer:
No Major Change in CRP/ESR: A pilot study found no significant shift in inflammatory markers such as C-reactive protein
(CRP) or erythrocyte sedimentation rate (ESR).
Lower Blood Counts: Hemoglobin (Hb), hematocrit (Ht), RBC, and WBC levels dipped during and just after Ramadan,
suggesting an increased risk of anemia—possibly from reduced iron, folic acid, or vitamin B12 intake.
5. What are the potential therapeutic benefits of intermittent hypoxia training?
Answer:
Hormonal Balance: May lower cortisol and ghrelin while boosting dopamine, GABA, melatonin, oxytocin, beta-endorphins,
anandamide, and serotonin.
Brain Health: Can raise brain blood flow (up to 20%), encourage neurogenesis, and defend against neurological decline.
Metabolic & Inflammatory Improvements: Helps regulate glucose metabolism, lower inflammation, and enhance
antioxidant levels.
Mood & Consciousness: Relieves anxiety, improves mood, and can induce euphoric or spiritual experiences, potentially
raising pain tolerance.
6. Which methods induce therapeutic hypoxia?
Answer:
Breath Control: Breath-retention exercises (e.g., Kumbhaka pranayama) or prolonged exhalation.
Blood Flow Restriction (BFR): Using a tourniquet or cuff during exercise to create localized hypoxia.
Chanting: Rhythmic vocalization can produce temporary oxygen deprivation.
Hypoxic Gas Mixtures: Face masks or chambers delivering low-oxygen air.
Rebreathing: Techniques like breathing into a paper bag to reduce oxygen temporarily (often for managing panic).
7. How do digital technologies support low-oxygen training and monitoring?
Answer:
Monitoring Devices: Pulse oximeters and wearable apps track oxygen levels in real time, issuing alerts if necessary.
Breathing Apps: Offer guided hypoxic exercises, featuring HRV analysis for stress and mood improvements.
Visualization & Gamification: Animated visuals encourage consistent breathing, while in-app rewards sustain motivation.
VR Biofeedback: Virtual reality systems provide immersive, real-time feedback for respiration control.
Telehealth & Specialized Equipment: Remote sessions via wireless sensors and advanced “hypoxicators” ensure safety and customization.
8. What are the challenges of home oxygen therapy, especially for families with infants?
Answer:
Equipment Size/Noise: Concentrators can be large, noisy, and emit heat, making certain areas uncomfortable.
Cannula Placement: Infants often resist nasal cannulas; running tubing under clothing or applying it during sleep may help.
Long Tubing Hazards: Extra-long tubing can get tangled or cause trips; secure the first few feet to the floor.
Weaning Delays: Home-based care may delay formal sleep studies or medical reviews needed to lower oxygen usage.
Alarm Fatigue: False alarms from pulse oximeters can create anxiety; high-quality probes may be more reliable.
Daily Life Adjustment: Tanks and monitors complicate errands and outings, though many manage near-normal routines.
Support Systems: Home nursing visits, online communities, and hotlines (e.g., American Lung Association) offer vital
Dr. Hassan Alwarraqi – Physician and medical researcher at h-k-e-m.com, dedicated to simplifying medical information and offering practical, compassionate care solutions.
Blends scientific knowledge with real-world experience to guide patients toward effective treatments like home oxygen therapy, restoring health, independence, and hope.
Keywords:
oxygen at home,
chronic respiratory disease,
breathing support,
oxygen concentrator,
COPD treatment,
hypoxemia management,
supplemental oxygen,
home healthcare,
patient hope,
respiratory therapy,
improve breathing at home.