Health is a crown on the heads of the healthy that only the sick can see.

🧠📈 Idiopathic Intracranial Hypertension (IIH) and Voluntary Fasting 🌙
Can voluntary fasting help relieve the symptoms of raised intracranial pressure (IIH)? Learn about the relationship between fasting, autophagy, improved brain health, and weight.
NERVOUS SYSTEM
Dr Hassan Al Warraqi
7/10/2025


🧠📈 Idiopathic Intracranial Hypertension (IIH) and Voluntary Fasting 🌙
Can voluntary fasting help relieve the symptoms of raised intracranial pressure (IIH)? Learn about the relationship between fasting, autophagy, improved brain health, and weight.
Intracranial Hypertension (IIH)
Definition and Other Names: Intracranial hypertension (IIH), formerly known as benign intracranial hypertension (BIH) or pseudotumor cerebri (PTC),
is a condition characterized by increased pressure within the skull without a tumor or other known cause.
Despite its former "benign" name, it is not benign and can lead to serious complications if left untreated, including permanent vision loss or blindness.
This condition occurs when the cerebrospinal fluid (CSF) surrounding the brain and spinal cord does not drain properly, leading to a buildup of pressure.
Causes and Risk Factors: The exact cause of intracranial hypertension is still unknown ("idiopathic" or "idiopathic").
However, several risk factors are associated with its development:
Gender and Age: It most commonly affects women between the ages of 20 and 50, with women affected approximately 20 times more often than men.
Before puberty, it occurs equally between boys and girls.
Obesity and Overweight: The most prominent risk factor.
Being overweight is associated with increased rates of IIH incidence or recurrence, and the disease improves with weight loss.
Women whose weight is more than 10% of their ideal body weight are thirteen times more likely to develop IIH, and this risk increases to nineteen times in women whose weight is more than 20% of their ideal body weight.
Medications: Certain medications can increase the risk of IIH, such as:
Tetracycline antibiotics (such as minocycline).
High-dose vitamin A derivatives (such as isotretinoin and retinoic acid).
Growth hormone.
Lithium.
Some oral contraceptives (although some sources suggest no clear association).
Corticosteroids (when starting or stopping).
Sulfa antibiotics.
Amiodarone, cyclosporine, cytarabine, levothyroxine (for children), nalidixic acid, nitrofurantoin, phenytoin, tamoxifen.
Hormonal imbalances: such as excessive levels of certain hormones, such as estrogen or corticosteroids, or polycystic ovary syndrome.
Underlying medical conditions: Obstructive sleep apnea.
Hypothyroidism.
Some autoimmune disorders (such as systemic lupus erythematosus and Behçet's disease).
Chronic kidney failure.
Down syndrome, Turner syndrome.
Iron deficiency anemia.
Some infections (such as HIV/AIDS, Lyme disease, after chickenpox in children).
Venous stenosis of the cerebral sinuses, especially the transverse sinus.
Pathophysiology (Mechanism): The exact mechanism of IIH development is not fully understood, but the following factors are believed to play a role:
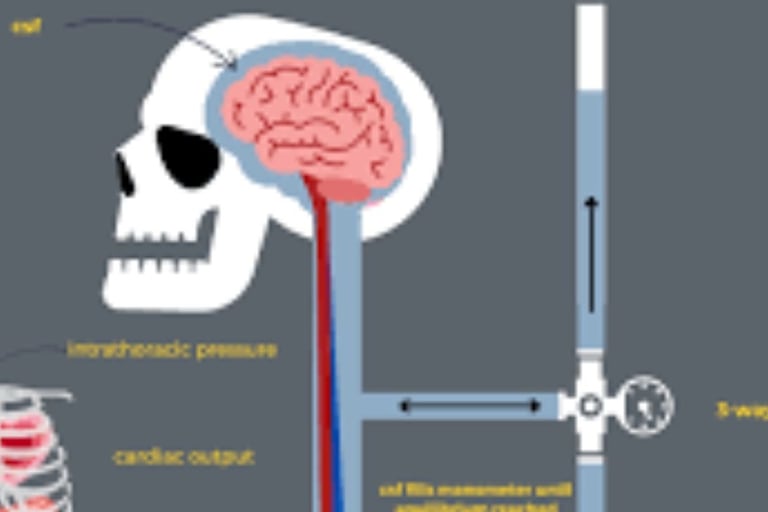
Cerebrospinal fluid (CSF) dynamics: There may be an imbalance between CSF production and absorption, leading to its accumulation.
Increased sinus venous pressure: Stenosis of the transverse venous sinuses is often observed in patients with IIH.
Increased sinus venous pressure may reduce CSF absorption.
Hormonal and metabolic factors: Elevated leptin levels in obese patients increase CSF secretion in the choroid plexus.
Symptoms and signs: Symptoms vary from person to person, but often include:
Severe headache: This occurs in approximately 90-94% of cases.
It is often described as throbbing, worse in the morning or with positional changes, or worsened by activities that increase intracranial pressure, such as coughing or sneezing.
It may be accompanied by nausea and vomiting.
The pain may be concentrated in the forehead or behind the eye, or it may be generalized throughout the head.
It can mimic a migraine in up to 70% of cases.
Visual disturbances: Affect more than 70% of patients.
Papilledema: Swelling of the optic nerve where it enters the eyeball, occurring in almost all cases of IIH.
It can lead to permanent vision loss if left untreated.
Transient visual obscurations: Recurrent episodes of partial blurring or dimming of vision in one or both eyes, lasting less than a minute, and triggered by position changes or Valsalva maneuvers.
Diplopia: Occurs in approximately 30% of patients, often horizontal, due to involvement of the sixth cranial nerve (abducens nerve).
Visual field loss: Often in peripheral vision, it may only be noticed by visual field tests.
Photophobia: Sensitivity to light.
Pulsatile tinnitus: A ringing or "whooshing" sound in one or both ears that coincides with the heartbeat, occurring in more than half of patients (64-87%).
Neck, shoulder, and back pain: occurs in approximately 42-53% of cases.
Nausea and vomiting.
Dizziness/vertigo.
Cognitive disturbance.
Tingling in the extremities, generalized weakness, or facial numbness.
Rarely, the facial nerve is affected, resulting in partial or complete weakness of the facial expression muscles.
Diagnosis
Diagnosis of IIH requires a careful assessment of symptoms and medical history and exclusion of other causes of increased intracranial pressure.
Comprehensive neurological examination: This includes assessment of vision, eye movements, and reflexes to look for any abnormalities.
Neuro-ophthalmological examination: This includes direct fundus examination, visual acuity measurement, pupillary examination, visual field examination, and optical coherence tomography (OCT) to evaluate papilledema.
Neuroimaging: Magnetic resonance imaging (MRI) or brain computed
tomography (CT) scan: This is necessary to rule out mass lesions (such as tumors) or other causes of elevated pressure.
In IIH, these tests usually show a diagnosis of glaucoma.
It is usually present, but signs such as partial or complete empty sella syndrome, flattening of the posterior globe, or optic nerve torsion may be present.
MRI or CT venography: Mandatory to rule out cerebral venous sinus thrombosis or transverse venous sinus stenosis, which are characteristic of many cases of IIH.
Lumbar puncture (spinal tap): This is the definitive diagnostic method. Cerebrospinal fluid (CSF) opening pressure is measured, which is usually elevated (greater than 250 mm Hg in adults or 280 mm Hg in obese children).
The CSF composition (protein, glucose, and cell count) should be normal.
Some fluid may be removed to temporarily relieve the pressure.
Diagnostic criteria: Based on the Modified Dandy Criteria or the International Classification of Headaches (ICHD-3) criteria, which require symptoms of elevated pressure, the absence of focal neurological signs (except for sixth nerve palsy), the patient being awake and alert, normal brain imaging without evidence of thrombosis, elevated CSF pressure with normal structure, and no other explanation for the elevated pressure.
Treatment
Treatment aims to relieve symptoms and prevent progression of optic nerve damage, primarily to preserve vision and reduce headache.
Lifestyle modifications: Weight loss: The only treatment that alters the course of the disease in IIH.
It is the recommended first-line treatment in the absence of sudden vision loss.
A weight loss of 6-10% can improve symptoms, and bariatric surgery shows promising results in achieving significant and lasting weight loss.
A healthy diet, reduced salt intake, and regular exercise.
Stress management.
Pharmacological treatment: Acetazolamide (Diamox): The most commonly used medication.
It works by reducing the production of cerebrospinal fluid by the choroid plexus.
The optimal dose is unknown, but it often starts at 250-500 mg twice daily and is gradually increased.
Common side effects include tingling in the fingers and toes, diarrhea, taste disturbances, fatigue, nausea, and, rarely, kidney stones. It is not recommended during pregnancy due to potential fetal risks.
Topiramate: May have a role, especially in cases of IIH accompanied by migraine.
It inhibits carbonic anhydrase and may reduce appetite and aid in weight loss.
Women should be warned that it may reduce the effectiveness of oral contraceptives and has a risk of fetal malformations.
Furosemide: It can be added to acetozolamide to enhance its diuretic effect, but it is not recommended as a sole treatment.
Painkillers: Nonsteroidal anti-inflammatory drugs (NSAIDs) and paracetamol can be used for headaches in the first weeks after diagnosis.
Indomethacin may have an advantage in reducing intracranial pressure.
Opioids are not recommended.
New Drugs: Recent promising studies have shown the effectiveness of drugs such as GLP-1 receptor agonists (such as exenatide) and 11-beta-hydroxysteroid dehydrogenase type 1 (11ß-HSD1) inhibitors in reducing intracranial pressure.
Repeated lumbar puncture: Not recommended as a long-term treatment strategy due to its short-term effect and associated risks such as pain and infection, but may be used as a temporary measure in severe cases or during pregnancy.
Surgical interventions: Considered in severe cases or when other treatments fail to protect vision or relieve symptoms.
Cerebrospinal fluid shunting (CSF shunting): This involves implanting a tube (catheter) to divert excess cerebrospinal fluid from the brain or spinal cord to another body cavity for absorption (often the abdomen).
The most common is the ventriculoperitoneal (VP) shunt, which is preferred over the lumboperitoneal (LP) shunt due to its lower revision rates.
Valves (pressure-constant or adjustable) are used to control fluid flow.
It is the most common choice for emergency surgery in cases of threatened vision loss.
Common complications include obstruction, infection, or overdrainage, which may require revision.
Optic Nerve Sheath Fenestration (ONSF): An opening is made in the optic nerve sheath behind the eye to reduce pressure on the nerve sheath, reducing papilledema and improving visual function.
It is less commonly used in the UK than in Europe and the US.
It is considered effective in improving vision, but less effective in relieving headaches.
Venous Sinus Stenting: This may be considered for patients with transverse venous sinus stenosis with a high pressure gradient.
It is believed to reduce venous hypertension, facilitating CSF absorption.
Its role is still being researched and not fully established.
Prevention
Preventive measures include:
Maintaining a healthy lifestyle: a balanced diet, regular physical activity, and managing weight within a healthy range.
Regular eye exams: to detect any changes in vision or papilledema early.
Caution with certain medications: Consult a doctor before starting or changing any medications known to increase the risk of IIH.
Stress management: Stress is thought to be a trigger for the condition.
Possible Complications
The most significant and serious complication of IIH is permanent vision loss or blindness if left untreated or poorly managed.
Some patients may experience chronic headaches despite controlled intracranial pressure.
Rare complications may include cerebral venous sinus thrombosis, cerebral hemorrhage, and subdural hematoma.
Prognosis
The course of IIH is variable.
The condition may sometimes resolve spontaneously within 6 months.
Symptoms may recur in some people. Symptoms may slowly worsen in a small number of people.
It can lead to blindness.
IIH does not usually affect life expectancy.
The most serious complication of idiopathic intracranial hypertension is permanent vision loss.
Therefore, regular follow-up with neurologists and ophthalmologists is crucial to monitor vision and adjust the treatment plan as needed.
Living with this condition requires adherence to the treatment plan, lifestyle changes, especially maintaining a healthy weight, and reporting any changes in symptoms to the doctor immediately.
Although the condition can be chronic for some, many patients are able to control their symptoms and preserve their vision with appropriate treatment and follow-up.
Important Notes:
If you suspect that you or someone else has intracranial hypertension, it is crucial to seek immediate medical attention by calling emergency services or consulting a neurologist.
The terms "benign" and "pseudotumor" are derived from the fact that elevated intracranial pressure may be associated with brain tumors.
Therefore, people in whom no tumor was found were diagnosed with "pseudotumor cerebri" (a disease that mimics a brain tumor).
The name of the disease was changed to benign intracranial hypertension in 1955 to distinguish it from intracranial hypertension caused by life-threatening conditions (such as cancer).
However, this name was also considered misleading because any condition that could lead to blindness should not be considered benign.
Therefore, the name was modified in 1989 to "idiopathic intracranial hypertension."
Idiopathic intracranial hypertension and the role of voluntary fasting
Benign intracranial hypertension (BIH) is a condition characterized by increased pressure within the skull without the presence of a tumor or other underlying disease.
Although the exact cause remains unclear, this condition is often associated with factors such as obesity, certain medications, and hormonal disorders.
Treatment for BIH involves a combination of medical therapies, lifestyle changes, and, in some cases, dietary interventions.
Voluntary fasting is emerging as a potential treatment for this condition. Research suggests that intermittent fasting, in particular, may offer several benefits that can help alleviate the symptoms of BIH, including:
Reducing inflammation: Fasting may help reduce inflammatory markers in the body, which may contribute to increased intracranial pressure.
This may lead to relief from symptoms associated with BIH.
Weight management: Since obesity is a major risk factor for BIH, voluntary fasting can aid weight loss.
Reducing body fat may relieve pressure on the brain, thus helping manage the condition.
Improving hormonal balance: Fasting helps regulate insulin levels and improve hormonal balance, which may be beneficial for people with BIH, as hormonal fluctuations are known to be a contributing factor.
Autolysis and cell health: Voluntary fasting stimulates autophagy, a natural process by which the body clears damaged cells.
This process may have a positive impact on brain health and alleviate symptoms associated with intracranial pressure.
Although voluntary fasting holds great promise, it is important to approach it with caution and under medical supervision.
Fasting is not a one-size-fits-all solution, and health conditions such as BIH may require customized management plans.
Ultimately, while voluntary fasting may offer potential benefits in managing BIH, it should be considered part of a comprehensive treatment approach that combines medical care, lifestyle changes, and dietary modifications to achieve the best results.
Frequently Asked Questions About Idiopathic Intracranial Hypertension (IIH) and the Role of Voluntary Fasting
What is idiopathic intracranial hypertension (IIH) in brief?
Idiopathic intracranial hypertension (IIH) is a condition in which the pressure around the brain increases without an obvious cause, such as a tumor or other disease.
This pressure can cause serious symptoms such as severe headaches and vision problems.
Is this condition serious?
Yes, it can be serious. The greatest risk is the potential for permanent damage to the optic nerve, which can lead to irreversible vision loss.
Therefore, early diagnosis and prompt treatment are essential.
Who is most at risk for this disease?
Women who are overweight or obese and of childbearing age (between 20 and 50 years old) are the most affected group.
Can men or children develop the disease?
Yes, although less common, men, children, and women outside the usual age range can also develop the disease.
What are the main symptoms I should look for?
Headache: Usually severe, worsening upon waking or lying down.
Vision problems: Such as blurred vision, double vision, brief episodes of blindness, or loss of peripheral vision.
Pulsatile tinnitus: A heartbeat-like sound is heard in one or both ears.
How is the disease diagnosed?
Diagnosis depends on ruling out other causes.
The main steps are:
Eye examination: To look for swelling of the optic nerve.
Brain imaging (magnetic resonance imaging) (MRI): To check for a tumor or other problems.
Lumbar puncture (spinal needle): To measure cerebrospinal fluid pressure and confirm it is elevated.
Does weight loss really help?
Yes, significantly. Weight loss is the most effective treatment for many overweight patients.
A small loss (5-10%) of body weight can significantly reduce pressure or even lead to complete recovery.
What treatments are available besides weight loss?
Medication: A medication such as acetazolamide (Diamox) is most commonly used to reduce cerebrospinal fluid production.
Surgery: This is used in severe cases or when vision is rapidly deteriorating, and includes procedures to reduce the pressure.
Relieving pressure on the optic nerve or implanting a shunt to drain excess fluid.
Will I need lifelong treatment?
This varies from person to person.
Some patients enter remission after losing weight and may not require ongoing treatment.
For others, the condition can be chronic and require long-term management and regular follow-up.
Can the disease recur after recovery?
Yes, there is a possibility of symptoms returning, especially if weight gain resumes.
Therefore, it is important to maintain a healthy lifestyle and follow up on any new symptoms with a doctor.
Can I exercise with this condition?
In general, yes. Low-impact exercise is very beneficial for helping to lose weight and improve overall health.
However, you should consult your doctor before starting any exercise program, as some activities that involve straining or bending excessively can temporarily aggravate headaches.
Is there a specific diet to follow?
There is no magic diet, but a balanced, low-calorie diet is recommended to aid weight loss.
Some people find that reducing their salt (sodium) intake helps reduce fluid retention and relieve symptoms.
What is the role of voluntary fasting in managing idiopathic intracranial hypertension (IIH)?
Voluntary fasting, may help manage IIH by:
Reducing inflammation in the body, which may contribute to lowering intracranial pressure.
Regulating weight, which is important as obesity is a major risk factor for IIH.
Improving hormonal balance and regulating insulin levels, which can contribute to reducing symptoms.
Stimulating autophagy, which can help reduce cell damage and improve overall health.
Is voluntary fasting safe for people with idiopathic intracranial hypertension?
Although voluntary fasting can have potential benefits, it should be done under medical supervision.
People with IIH should consult a doctor before starting any fasting regimen, especially if they are taking medications or have other medical conditions that may be affected by fasting.
Does fasting help relieve symptoms in the long term?
While fasting may help improve some symptoms, such as headaches or nerve inflammation, its long-term effects still require further scientific research.
It is important to consider fasting as part of a comprehensive treatment plan that includes ongoing medical care.
What are some tips for practicing fasting safely with idiopathic intracranial hypertension?
Consult your doctor before starting any fasting regimen.
Start with intermittent fasting or short-term fasting before expanding to longer periods.
Ensure you eat a healthy, balanced diet during fasting periods.
Maintain adequate hydration to avoid any adverse effects on the brain.
Avoid fasting if you have any severe or emergency symptoms.
Can fasting replace medical treatment for idiopathic intracranial hypertension?
No, fasting is not considered a substitute for medical treatment.
Fasting should be part of a comprehensive plan that includes medications and other treatments recommended by your doctor.
Hassan Al-Waraqi is a health content creator and founder of H-K-E-M.com, a platform focused on providing educational content for people about idiopathic intracranial hypertension (IIH).
Through his platform, Hassan provides comprehensive guides on how to manage IIH, including lifestyle changes, dietary modifications, and alternative treatments.
His commitment to providing scientific and research-backed medical content aims to support people with IIH, helping them understand their condition and find ways to improve their quality of life.