Health is a crown on the heads of the healthy that only the sick can see.

🦴 Rheumatoid Arthritis (RA): A Multidisciplinary Approach 🩺💪
Discover how a multidisciplinary approach—combining rheumatology, nutrition, physical therapy, and mental health—can improve quality of life for people with Rheumatoid Arthritis (RA). Explore holistic care strategies on H-K-E-M.com.
AUTOIMMUNE DISEASES
Dr Hassan Al warraqi
12/11/2024


🦴 Rheumatoid Arthritis (RA): A Multidisciplinary Approach 🩺💪
Understanding Rheumatoid Arthritis: Causes, Symptoms, and Treatments
Fasting and Rheumatoid Arthritis
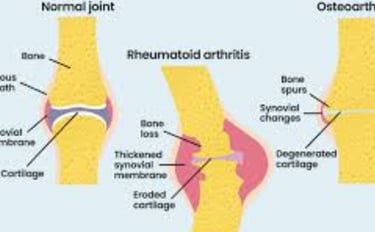
Rheumatoid arthritis (RA) is a chronic autoimmune condition affecting millions globally. It primarily targets the joints, causing inflammation, pain, and potential joint damage if untreated.
Unlike osteoarthritis, which stems from wear and tear, RA results from an immune system malfunction that mistakenly attacks healthy tissues.
This article delves into the causes, symptoms, diagnosis, and treatment options for RA, offering insights to empower individuals in managing this life-altering disease.
What is Rheumatoid Arthritis?
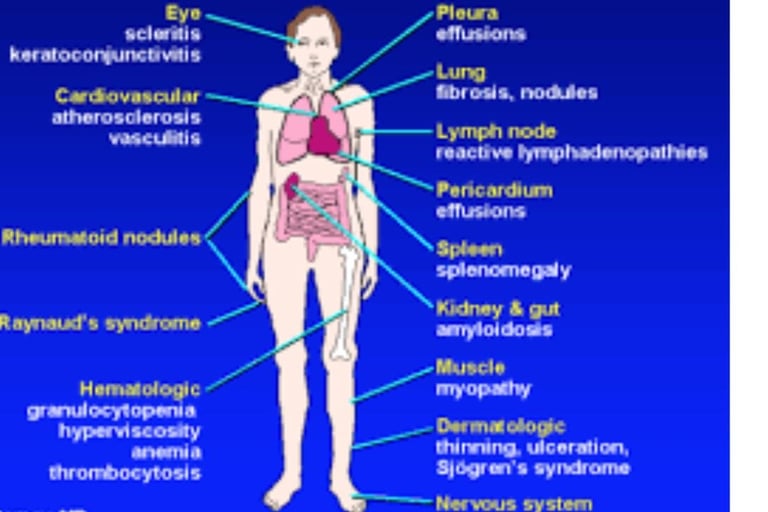
RA is a systemic disorder that extends beyond the joints, potentially affecting the heart, lungs, eyes, and skin.
Characterized by flare-ups and periods of remission, the condition primarily targets the synovium, the joint-lining tissue, leading to bone and cartilage erosion over time.
Epidemiology
RA affects about 1% of the global population, with women being three times more likely to develop it than men. It typically begins between ages 30 and 60 but can occur at any age.
Causes and Risk Factors
RA arises from an interplay of genetic, environmental, hormonal, and immune factors:
Genetics: Specific markers like HLA-DR4 increase susceptibility.
Environmental Triggers: Smoking and exposure to certain toxins or infections can activate the condition in predisposed individuals.
Hormonal Influences: Hormones like estrogen may play a role, as RA often improves during pregnancy and flares postpartum.
Immune Dysfunction: The immune system's mistaken attack on the synovium leads to inflammation and damage.
Symptoms
RA manifests with joint-specific and systemic symptoms:
Joint Symptoms: Pain, swelling, and morning stiffness lasting over 30 minutes.
Systemic Symptoms: Fatigue, fever, appetite loss, and weight loss.
Advanced Symptoms: Joint deformities and rheumatoid nodules.
Extra-Articular Manifestations: Complications affecting the lungs, heart, and eyes.
Diagnosis
RA is diagnosed through clinical evaluation, laboratory tests, and imaging studies:
Clinical Evaluation: Assessing joint swelling, tenderness, and mobility.
Laboratory Tests: Anti-CCP antibodies, RF, ESR, and CRP levels indicate inflammation.
Imaging: X-rays, ultrasounds, or MRIs identify joint damage and inflammation.
Early Stages of Rheumatoid Arthritis (RA)
The initial phases of RA are crucial for timely diagnosis and treatment, as early intervention can significantly alter the disease's progression.
Stage 1: Early RA
In the first stage, referred to as Early RA, patients often present with mild symptoms, including joint pain and slight swelling, typically in smaller joints like the hands and feet. Prompt identification at this stage can greatly improve treatment outcomes.
Symptoms
Early RA symptoms may be subtle but are key indicators for early detection, which is essential for effective management:
Mild joint pain, often mistaken for muscle fatigue or aging-related discomfort
Slight swelling in smaller joints, such as fingers and toes
General fatigue or a feeling of being unwell
Diagnosis
Diagnosis during this stage relies on:
Blood Tests: Detecting markers like rheumatoid factor (RF) and C-reactive protein (CRP)
Imaging Tests: X-rays or MRIs to identify early joint damage
Early diagnosis is vital to prevent long-term complications.
Stage 2: Antibody Formation and Mild RA
In Stage 2, the immune system starts producing antibodies, such as RF, leading to more persistent symptoms and increased joint inflammation.
Symptoms
At this stage, symptoms become more noticeable and may extend to larger joints:
Persistent joint pain that is harder to dismiss
Pronounced joint swelling, often noticeable after waking
Morning stiffness and reduced range of motion in affected joints
Diagnosis
Blood Tests: Increasing importance for detecting elevated RF levels and other inflammatory markers
Imaging Tests: Continued use to assess progression and rule out other conditions
Early treatment during this phase can slow the disease's advancement.
Later Stages of Rheumatoid Arthritis
As RA progresses, symptoms intensify, and joint damage becomes more significant, impacting both form and function.
Stage 3: Moderate RA
In this stage, inflammation becomes severe, and joint damage starts to affect daily activities. Rheumatoid nodules, firm lumps beneath the skin, may also appear.
Symptoms
Severe joint pain and inflammation
Formation of visible rheumatoid nodules, especially near the elbows and hands
Carpal tunnel syndrome caused by wrist inflammation
Imaging studies revealing clear joint damage
Diagnosis
Blood Tests: High levels of inflammatory markers like CRP and RF
Imaging Studies: Evident joint erosion and damage
At this stage, the diagnosis is more apparent due to the severity of symptoms.
Stage 4: Severe RA
The final stage of RA is characterized by extensive joint damage, deformities, and significant limitations in mobility. This stage has a profound impact on the patient’s quality of life.
Symptoms
Intense joint pain and chronic inflammation
Severe deformities in the joints
Loss of joint function and significant mobility restrictions
Surgical Interventions
For those in Stage 4, surgical procedures, such as joint replacements or repairs, may be necessary to restore physical function and alleviate symptoms.
Understanding the Four Stages of RA
RA progresses through distinct stages, each marked by worsening symptoms and joint damage. Early detection and treatment are critical in slowing the disease and improving quality of life.
Treatment Options
A multidisciplinary approach is essential for managing RA effectively:
Medications:
DMARDs: Slows disease progression (e.g., methotrexate).
Biologics: Target immune system components (e.g., adalimumab).
JAK Inhibitors: Block inflammatory pathways.
NSAIDs and Corticosteroids: Reduce pain and inflammation during flare-ups.
Lifestyle Changes:
Regular low-impact exercises like yoga.
Anti-inflammatory diets rich in fruits, vegetables, and omega-3s.
Stress management through mindfulness or relaxation techniques.
Smoking and alcohol cessation.
Surgical Options:
Synovectomy, joint replacements, or tendon repairs for severe cases.
Living with Rheumatoid Arthritis
Managing RA involves medical, lifestyle, and emotional strategies:
Emotional Support: Joining support groups and seeking therapy.
Disease Monitoring: Regular check-ups and symptom tracking.
Workplace Adjustments: Ergonomic setups and flexible schedules.
Research and Innovations
Advances in precision medicine and biologics are paving the way for tailored therapies, offering hope for improved RA management.
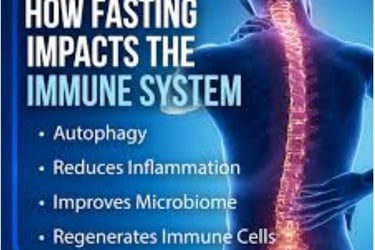
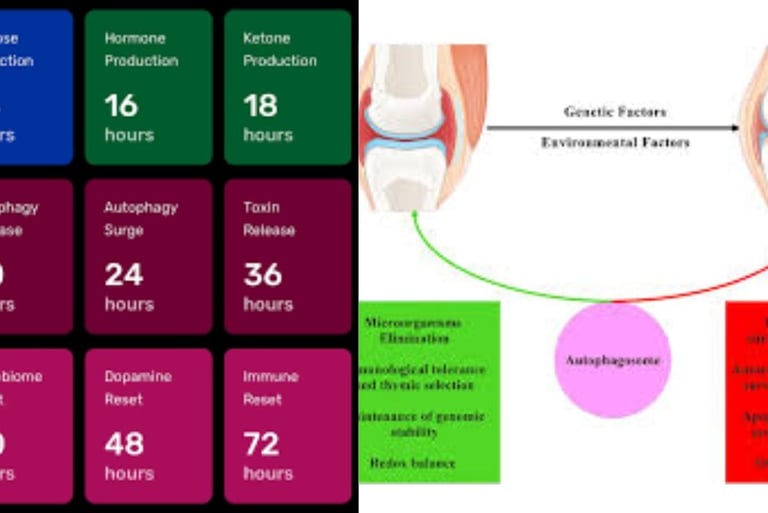
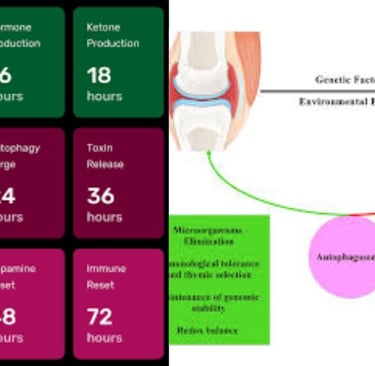
Fasting and Rheumatoid Arthritis: Exploring Potential Benefits
Recent research highlights fasting as a complementary approach for RA management, showing potential to reduce inflammation and modulate immune responses.
Mechanisms of Fasting
Inflammatory Modulation: Reduces cytokines like TNF-α and IL-6.
Immune Reset: Enhances autophagy, clears damaged cells, and reduces autoantibody production.Potential "reset" of immune system dysfunction.
Gut Microbiome Impact: Improves gut-immune interactions by altering microbiota.
Shifts from glucose to ketone metabolism
Evidence from Clinical Studies
Fasting reduces disease activity scores, pain, and stiffness.
Sustained symptom relief observed in some studies.
80% of patients experienced improved symptoms
Sustained benefits for several months after fasting period
Reduced inflammatory markers
Types of Fasting
Intermittent Fasting: Flexible and sustainable.
Prolonged Fasting: Intense but requires supervision.
Fasting-Mimicking Diet: Combines benefits of fasting with minimal caloric intake.
islamic fasting : 3 days per month white days ,monday and thursday ,alternative day or david fasting and lastly fast everyday except friday.
Considerations
Fasting may not suit everyone.
Risks include nutritional deficiencies and hormonal disruptions.
Always consult healthcare providers before starting fasting interventions.
Females are more commonly affected by rheumatoid arthritis (RA) due to a combination of hormonal, genetic, and immunological factors
Several key factors contribute to this gender disparity
1. Hormonal Influences :
- Estrogen and other sex hormones play a role in immune regulation. Variations in these hormones may predispose women to an overactive immune response, contributing to autoimmune conditions like RA.
- RA often improves during pregnancy (when hormonal balance shifts) and flares postpartum, suggesting a strong link to hormonal changes.
worsens during hormonal shifts, such as:
* After pregnancy
* During perimenopause
* Around menopause
2. Genetic Susceptibility :
- Specific genetic markers, such as HLA-DR4, associated with RA, are more frequently expressed in women, potentially increasing their risk.
3. Immune System Differences :
- Women's immune systems are generally more robust and active than men’s, which is advantageous for fighting infections but may also increase the likelihood of autoimmune conditions like RA.
4. Environmental and Lifestyle Factors :
- Smoking and hormonal changes related to pregnancy, menopause, or hormonal therapies may further contribute to the increased prevalence of RA in women.
5. Epigenetic Factors
- Hormonal and environmental influences can cause epigenetic modifications
- These modifications may alter gene expression related to immune system functioning
- Such changes can potentially increase susceptibility to autoimmune conditions
These factors collectively make women approximately three times more likely to develop RA than men.
While these factors help explain the higher prevalence of RA in females, it's important to note that the exact mechanisms are still being researched.
The interplay between genetics, hormones, and immune system responses creates a complex landscape that makes women more vulnerable to this complication.
Current medical research continues to investigate these connections to develop more targeted treatments and understanding of RA's gender-specific manifestations.
chronic inflammatory disorder.
Conclusion
While fasting is not a standalone treatment, it shows promise as part of an integrative RA management plan.
Personalized guidance and further research are essential to harness its full potential.
This reframed content streamlines the original text while maintaining its comprehensiveness and clarity. Let me know if further adjustments are needed!
keywords
Rheumatoid Arthritis, chronic inflammation, joint pain, synovium damage, systemic disease features, joint damage, flare-ups, and periods of remission,fasting, inflammation, autoimmune, cytokine reduction, immune modulation, metabolic switching, autophagy, anti-inflammatory intervention, cellular repair, oxidative stress, immune system reset, nutritional therapy, clinical research, metabolic reprogramming, personalized medicine.
https://www.mayoclinic.org/diseases-conditions/rheumatoid-arthritis/symptoms-causes/syc-20353648
https://my.clevelandclinic.org/health/diseases/4924-rheumatoid-arthritis
https://www.arthritis.org/diseases/rheumatoid-arthritis
Questions and Answers About Rheumatoid Arthritis (RA) and Fasting
1. What is rheumatoid arthritis, and what factors increase the risk of developing it?
Rheumatoid arthritis (RA) is a chronic autoimmune disease that primarily affects the joints but can also impact other organs such as the heart, lungs, eyes, and skin.
It occurs due to a malfunction in the immune system, which attacks healthy body tissues.
Risk factors include genetic predisposition (e.g., HLA-DR4 markers), environmental exposures (e.g., smoking and toxins), hormonal influences (especially in women), and autoimmune factors.
Women are three times more likely to develop RA than men.
2. What are the early symptoms of rheumatoid arthritis, and how is it diagnosed in its early stages?
Early symptoms of RA include mild joint pain, particularly in small joints like the hands and feet, slight swelling, and general fatigue.
These symptoms can be mistaken for other conditions, such as muscle strain.
Diagnosis at this stage involves blood tests to detect markers like rheumatoid factor (RF) and C-reactive protein (CRP), along with imaging tests such as X-rays and MRIs to identify early joint damage.
3. How does rheumatoid arthritis progress, and what are the symptoms of each stage?
RA progresses through four stages:
Stage 1 (Early): Symptoms are mild.
Stage 2 (Formation of antibodies and mild inflammation): Symptoms become more pronounced, with persistent pain and swelling.
Stage 3 (Moderate): Inflammation becomes severe, rheumatoid nodules appear, and joint damage starts to affect daily activities.
Stage 4 (Severe): Joint damage becomes extensive, leading to deformities and significantly restricted movement.
4. What treatment options are available for managing rheumatoid arthritis?
Managing RA requires a multidisciplinary approach. Treatment includes:
Medications: Disease-modifying antirheumatic drugs (DMARDs) like methotrexate, biologics targeting specific immune components, JAK inhibitors, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids for pain and inflammation relief.
Non-drug therapies: Lifestyle changes such as light exercise, an anti-inflammatory diet, stress management, and quitting smoking.
Surgery: May be necessary in severe cases.
5. What is the relationship between fasting and rheumatoid arthritis, and how can fasting benefit people with RA?
Recent research suggests that fasting may have potential benefits in managing RA.
Fasting can reduce inflammation by lowering inflammatory cytokines such as TNF-α and IL-6, improving immune response, modulating gut microbiota, and promoting autophagy, which helps clear damaged cells.
Fasting may also shift metabolism from glucose utilization to ketone usage.
Clinical studies indicate fasting can alleviate symptoms, reduce pain and stiffness, and improve inflammatory markers.
6. What types of fasting may benefit rheumatoid arthritis, and what are the risks and considerations?
Beneficial fasting types include intermittent fasting, prolonged fasting (with supervision), and fasting-mimicking diets.
For Islamic fasting, practices like fasting on the white days of each month, Mondays and Thursdays, alternate days (David’s fast), or daily fasting except Fridays are possible options.
Individuals should consult healthcare providers before starting any fasting regimen.
Potential risks include nutritional deficiencies and hormonal imbalances, making it essential to tailor fasting to individual health conditions.
Fasting should be part of an integrated disease management plan rather than a standalone treatment.
7. Why are women more likely to develop rheumatoid arthritis than men?
Women are three times more likely to develop RA due to a combination of hormonal, genetic, and immune factors.
Hormones like estrogen play a role in immune system regulation, and hormonal changes may trigger an excessive immune response in women, increasing the risk of autoimmune diseases.
Additionally, certain genetic markers linked to RA are more common in women, and their immune systems tend to be more active overall, raising susceptibility to autoimmune conditions.
8. What are the latest advancements in rheumatoid arthritis research, and what role does precision medicine play in treatment?
RA research is continually advancing, particularly in precision medicine, which focuses on personalized treatments based on genetic and immune characteristics.
Research has enhanced understanding of the immune mechanisms driving the disease, paving the way for more effective therapies.
Innovations include biological drugs and treatments targeting specific inflammatory pathways to improve disease management and reduce complications.