Health is a crown on the heads of the healthy that only the sick can see.

Frequent fluid accumulation : fasting, honey and cold water
Explore the essential aspects of abdominal paracentesis, a vital procedure for diagnosing and treating conditions like ascites, cirrhosis, and malignancy. Learn about peritoneal fluid analysis, pot...
GASTROINTESTINAL
Dr Hassan Al Warraqi
11/28/2024

Frequent fluid accumulation in the abdomen: Benefits of fasting, honey and cold water
Abdominal Paracentesis: Diagnostic & Therapeutic Insights
Frequent fluid accumulation in the abdomen: Benefits of fasting, honey and cold water
Introduction to Abdominal Paracentesis
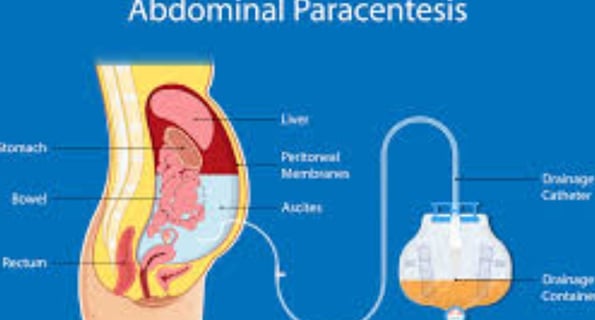
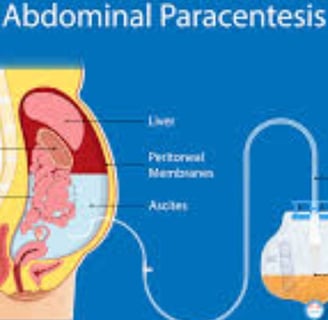
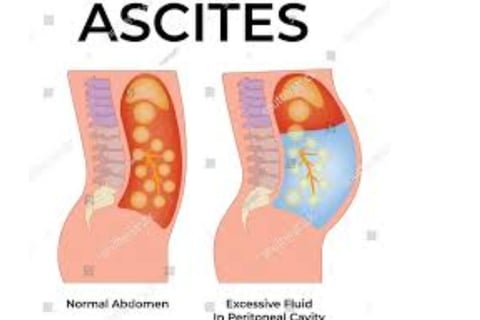
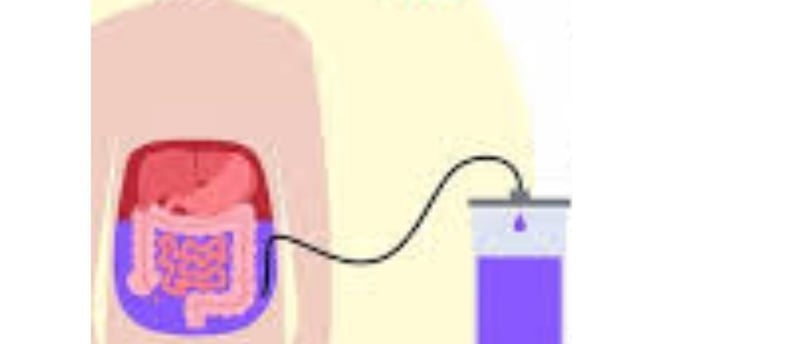
Abdominal paracentesis, also known as peritoneocentesis or laparocentesis, is a medical procedure where a needle or catheter is inserted into the peritoneal cavity to remove or sample peritoneal fluid.
This fluid can accumulate due to various conditions, most commonly ascites caused by liver cirrhosis.
The term "paracentesis" originates from the Greek word κεντάω, meaning "to pierce." This article delves into various aspects of abdominal paracentesis, from indications and procedure to potential complications.
What is Abdominal Paracentesis?
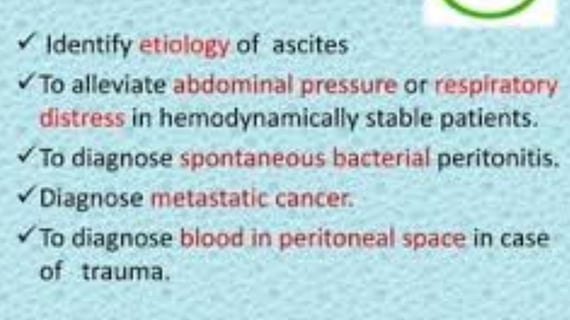
Abdominal paracentesis is both a diagnostic and therapeutic procedure. It serves two primary purposes:
Diagnostic: To analyze peritoneal fluid and determine its cause, such as infections, cancer, or other diseases.
Therapeutic: To relieve symptoms caused by excessive fluid accumulation, such as abdominal discomfort, breathing difficulties, or pressure.
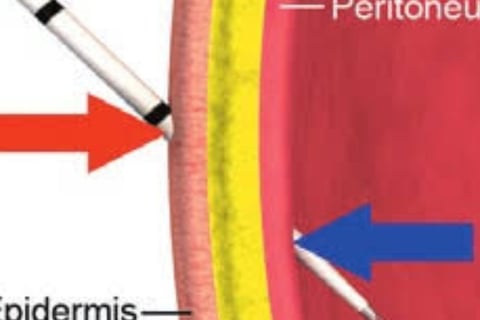
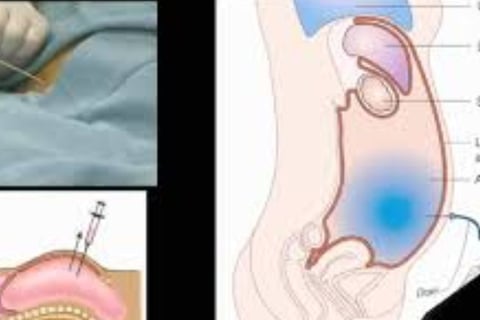
Where is the Site for a Paracentesis?
The site for abdominal paracentesis is typically chosen based on the location of the fluid accumulation. Common sites include:
Midline Approach: Two centimeters below the umbilicus, avoiding major blood vessels.
Lateral Approach: Two fingerbreadths medial and superior to the anterior superior iliac spine, on either side of the abdomen.
Ultrasound guidance is often used to ensure safety and precision.
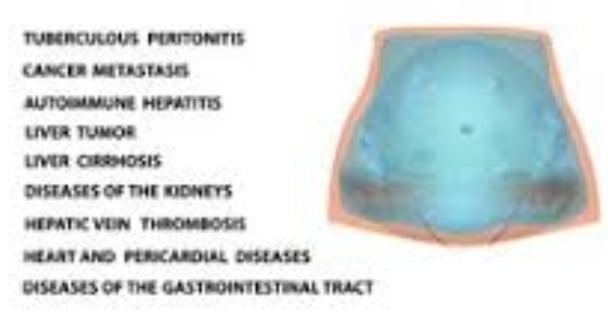
What are the Indications for Paracentesis?
Paracentesis is indicated in several conditions, primarily involving the diagnosis or treatment of peritoneal fluid buildup.
Common indications include:
Ascites Evaluation:
Cirrhosis-related ascites.
Malignancy-related ascites.
Suspected Peritonitis:
Spontaneous bacterial peritonitis (SBP).
Tuberculous peritonitis.
Relief of Symptoms:
Severe abdominal distension.
Respiratory compromise due to ascitic pressure.
Contraindications of Abdominal Paracentesis
While generally safe, paracentesis has some contraindications:
Absolute Contraindications:
Acute abdomen requiring surgical intervention.
Relative Contraindications:
Coagulopathy (INR > 2.0 or platelets < 50,000).
Pregnancy.
Prior abdominal surgeries with extensive adhesions.
How to Perform a Paracentesis?
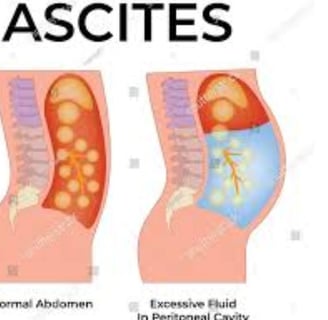
Preparation:
Patient Positioning: Supine position or slightly elevated (30-45 degrees) to allow fluid pooling.
Skin Preparation: Sterilize the area with antiseptic.
Procedure:
Identify the Site: Use clinical examination or ultrasound guidance.
Local Anesthesia: Administer lidocaine to numb the site.
Needle Insertion: Insert a needle or catheter into the peritoneal cavity at the identified site.
Fluid Aspiration: Collect fluid for diagnostic purposes or drain excess fluid for therapeutic reasons.
Post-Procedure: Apply a sterile dressing and monitor for complications.
Abdominal Paracentesis Purpose
The purpose of abdominal paracentesis can be categorized into diagnostic and therapeutic goals:
Diagnostic: To analyze fluid composition, including albumin, protein, cytology, and microbiology.
Therapeutic: To relieve symptoms of fluid overload, such as abdominal pain and respiratory distress.
Why Give Albumin After Paracentesis?
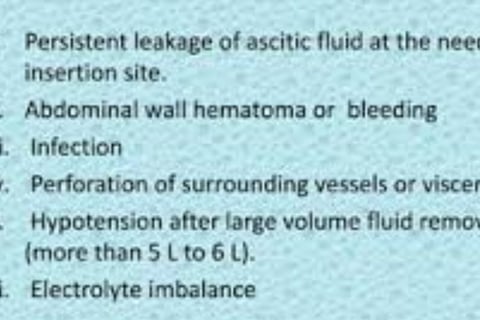
Large-volume paracentesis (removal of >5 liters of fluid) can lead to complications such as circulatory dysfunction. Albumin infusion helps to:
Maintain intravascular volume.
Prevent paracentesis-induced circulatory dysfunction (PICD).
Improve patient outcomes by reducing hypotension and kidney dysfunction risks.
What is the Best Position for Abdominal Paracentesis?
The best position for the procedure is typically the semi-Fowler's position, where the patient lies supine with the head elevated to 30-45 degrees.
This allows fluid to pool in the lower abdomen, making it easier to access.
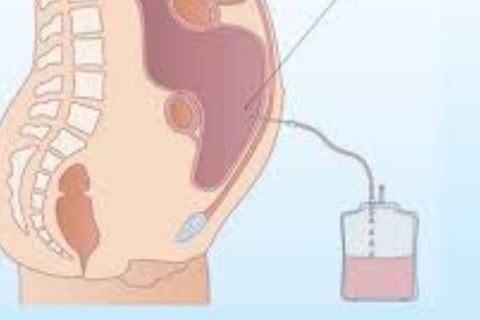
Complications of Abdominal Paracentesis
While generally safe, complications can occur:
Common Complications:
Bleeding or hematoma at the puncture site.
Infection or peritonitis.
Leakage of ascitic fluid.
reaccumulation of the fluid .
Rare Complications:
Bowel perforation.
Hypovolemia (especially after large-volume paracentesis).
Paracentesis-induced circulatory dysfunction (PICD).
Key Clinical Considerations in Paracentesis
Most Common Site for Ascitic Tap:
The infra-umbilical midline or the lateral lower quadrants are preferred for ascitic taps.
Difference Between Ascites and Paracentesis:
Ascites: The condition involving fluid accumulation in the peritoneal cavity.
Paracentesis: The procedure performed to remove or analyze this fluid.
Difference Between Peritoneal Fluid and Paracentesis:
Peritoneal Fluid: A natural lubricating fluid in the peritoneal cavity.
Paracentesis: The act of extracting excess or pathological fluid from the cavity.
Criteria for Ascitic Fluid Analysis:
Serum-Ascites Albumin Gradient (SAAG): Helps distinguish between transudative (e.g., cirrhosis) and exudative (e.g., malignancy) ascites.
Microbiological Analysis: For detecting infections such as SBP.
Cytology: For diagnosing cancer.
Abdominocentesis vs. Thoracentesis
Abdominocentesis: Targets fluid in the peritoneal cavity.
Thoracentesis: Removes fluid from the pleural cavity in the chest.
Technological Aids in Abdominal Paracentesis
Modern advancements, such as 3D animations, procedural videos, and ultrasound-guided techniques, have improved the accuracy and safety of abdominal paracentesis.
These resources are widely available to enhance medical education and patient understanding.
Conclusion
Abdominal paracentesis is a vital diagnostic and therapeutic tool in managing conditions like ascites.
With proper technique, careful patient selection, and attention to complications, it remains an effective and safe procedure.
Its role continues to evolve with advancements in technology and clinical practice, ensuring better patient outcomes.
Reaccumulation of the peritoneal fluid
Reaccumulation of Peritoneal Fluid: Causes, Management, and Implications
Reaccumulation of peritoneal fluid refers to the return of excess fluid within the peritoneal cavity following an initial removal, typically through a procedure like abdominal paracentesis.
This phenomenon is common in patients with chronic conditions that cause ascites and often signals an ongoing or unresolved underlying pathology.
Understanding its causes, implications, and management strategies is essential for effective patient care.
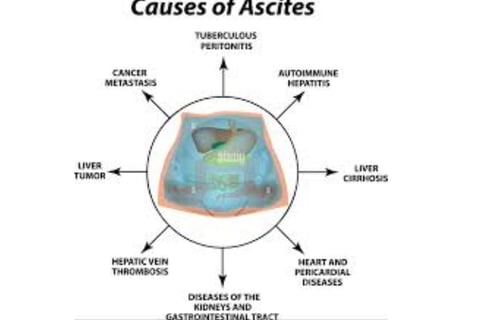
Causes of Reaccumulation of Peritoneal Fluid
Liver Cirrhosis (Portal Hypertension):
The most common cause of recurrent ascites.
Increased pressure in the portal venous system leads to fluid leakage into the peritoneal cavity.
Malignancy:
Peritoneal carcinomatosis or metastatic cancers can cause persistent fluid accumulation due to tumor-related inflammation and vascular permeability.
Heart Failure:
Congestive heart failure can lead to recurrent ascites due to systemic venous congestion.
Nephrotic Syndrome:
Hypoalbuminemia from kidney dysfunction reduces oncotic pressure, leading to recurrent fluid leakage.
Tuberculous Peritonitis:
Persistent infection in the peritoneum can lead to ongoing fluid accumulation.
Pancreatic Disorders:
Pancreatic ascites, due to leakage from pancreatic ductal disruptions, may reaccumulate without definitive management of the underlying cause.
Chylous Ascites:
Obstruction or trauma to the lymphatic system can cause ongoing chylous fluid production.
Implications of Reaccumulation
Patient Symptoms:
Persistent abdominal distension.
Pain or discomfort.
Dyspnea due to increased intra-abdominal pressure.
Compromised Quality of Life:
Frequent medical interventions (e.g., repeat paracentesis) can burden patients physically and emotionally.
Progression of Disease:
Reaccumulation may indicate worsening of the underlying condition, necessitating a reassessment of the treatment plan.
Risk of Complications:
Repeated paracentesis increases the risk of infections, protein loss, and electrolyte imbalances.
Management of Reaccumulation of Peritoneal Fluid
Treat the Underlying Cause:
Cirrhosis: Optimize management with diuretics (e.g., spironolactone, furosemide), salt restriction, and treatment of liver disease. Consider transjugular intrahepatic portosystemic shunt (TIPS) in refractory cases.
Malignancy: Use chemotherapy, targeted therapies, or palliative care based on the cancer type and stage.
Infections: Treat bacterial or tuberculous peritonitis with appropriate antibiotics or antitubercular therapy.
Dietary Modifications:
Sodium restriction (<2 grams/day) to reduce fluid retention.
Adequate protein intake to combat hypoalbuminemia.
Recurrent Paracentesis:
Necessary for symptomatic relief in refractory cases.
Often combined with albumin infusion to prevent circulatory dysfunction.
Use of Diuretics:
Diuretics can help reduce fluid accumulation but must be used cautiously to avoid kidney dysfunction or electrolyte imbalances.
Peritoneovenous Shunt:
An option for patients with refractory ascites when other treatments fail.
Consider Liver Transplantation:
For patients with advanced liver disease and recurrent ascites, transplantation may be the definitive solution.
Palliative Care:
In terminal cases, focus on symptom relief and quality of life through conservative management.
Monitoring and Prevention
Regular Follow-Up:
Monitor for signs of fluid reaccumulation, including weight gain and abdominal girth measurements.
Preventative Strategies:
Early management of conditions like cirrhosis, heart failure, or infections can reduce the likelihood of ascites recurrence.
Vaccination against hepatitis viruses to prevent liver disease progression.
Patient Education:
Teach patients to recognize symptoms of fluid reaccumulation and adhere to dietary and medication regimens.
Conclusion
Reaccumulation of peritoneal fluid poses significant challenges in managing patients with ascites.
A comprehensive approach addressing the underlying cause, optimizing medical therapy, and implementing appropriate interventions can improve outcomes and reduce the need for repeated procedures like paracentesis.
By integrating patient-centered care and multidisciplinary collaboration, healthcare providers can effectively manage this complex condition.
Fasting Outside Ramadan and Cold Water Therapy: The Role of Honey and Manuka Honey in Management
Fasting and therapeutic modalities like cold water therapy have garnered attention for their potential health benefits.
When combined with the therapeutic properties of natural substances like honey and Manuka honey, these practices may play a significant role in promoting health and managing various conditions.
Here, we explore how fasting outside Ramadan, cold water therapy, and honey contribute to holistic health.
Fasting Outside Ramadan: Benefits and Role in Management
Fasting outside of Ramadan, such as intermittent fasting or voluntary abstinence from food and drink for extended periods, or islamic fasting . offers numerous health benefits:
1. Metabolic Health:
Blood Sugar Regulation: Improves insulin sensitivity and lowers blood sugar levels, reducing the risk of type 2 diabetes.
Weight Management: Promotes fat metabolism, helping with weight loss and body composition improvements.
2. Cellular Repair and Longevity:
Fasting stimulates autophagy, a process where cells remove damaged components, potentially slowing aging and reducing the risk of chronic diseases.
3. Immune System Modulation:
Periodic fasting may reduce inflammation and support immune function, making it useful for managing autoimmune conditions.
4. Mental Clarity:
Enhances brain function by increasing levels of brain-derived neurotrophic factor (BDNF), which supports learning and memory.
Cold Water Therapy: Benefits and Role in Management
Cold water therapy, involving exposure to cold water through baths, showers, or immersion, has gained popularity for its therapeutic effects:
1. Anti-Inflammatory Effects:
Reduces inflammation, aiding in recovery from injuries and chronic inflammatory conditions like arthritis.
2. Improved Circulation:
Cold exposure stimulates blood flow and improves cardiovascular health.
3. Boosted Immune System:
Regular cold water exposure may enhance immune responses and resistance to infections.
4. Mental Health Benefits:
Can alleviate symptoms of anxiety and depression by triggering endorphin release and improving mood.
Honey and Manuka Honey in Management
Honey, particularly Manuka honey, is celebrated for its unique therapeutic properties due to its composition of natural sugars, enzymes, antioxidants, and bioactive compounds.
1. Wound Healing:
Antimicrobial Properties: Manuka honey is effective against various bacteria, including antibiotic-resistant strains, due to its high methylglyoxal (MGO) content.
Skin Repair: Promotes tissue regeneration and reduces infection risks in wounds and burns.
2. Digestive Health:
Gut Microbiome Support: Honey acts as a prebiotic, fostering beneficial gut bacteria.
Ulcer Management: Manuka honey may help heal gastric ulcers caused by Helicobacter pylori infection.
3. Immune System Support:
Antioxidant Effects: Boosts immunity by reducing oxidative stress and inflammation.
Cold and Flu Relief: Soothes sore throats and reduces cough severity.
4. Role in Metabolic Health:
Glycemic Control: While honey is a natural sugar, it has a lower glycemic index than refined sugars, making it a healthier alternative.
Energy Source: Provides sustained energy for fasting individuals due to its natural sugar content.
Combining Practices for Holistic Health
Fasting and Honey:
During fasting periods, consuming honey before or after the fast can provide quick energy, reduce inflammation, and support digestion.
Honey's antioxidant properties complement the cellular repair benefits of fasting.
Cold Water Therapy and Honey:
Cold water therapy reduces inflammation, while honey supports healing and immune response, making them synergistic in recovery and chronic condition management.
Manuka Honey as a Therapeutic Agent:
Manuka honey can be applied topically for skin conditions or consumed for internal health benefits, enhancing the effects of fasting and cold exposure.
Practical Tips for Incorporation
Fasting Protocols:
Start with intermittent fasting (16:8) and gradually increase fasting durations.
islamic fasting is agood choice
Use honey as a natural sweetener for tea or warm water post-fast to replenish energy.
Cold Water Therapy:
Begin with short cold showers or partial immersion and extend the duration as your body adapts.
Combine therapy with honey to boost recovery from cold-induced stress.
Manuka Honey Use:
Take 1–2 teaspoons of Manuka honey daily on an empty stomach for gut health.
Apply topically for wound care or mix with warm water for throat and immune support.
Conclusion
Fasting, cold water therapy, and the use of honey, particularly Manuka honey, form a complementary trio for managing health conditions and enhancing overall well-being.
Fasting promotes cellular repair and metabolic health, cold water therapy reduces inflammation and improves circulation, while honey provides essential nutrients and antimicrobial benefits.
Together, these practices support a natural and holistic approach to health management.
Frequently Asked Questions about Abdominal Paracentesis, Fluid Accumulation, Fasting, Cold Water Therapy, and Honey Treatment:
1. What is Abdominal Paracentesis, and what are its purposes?
Abdominal paracentesis is a medical procedure involving the insertion of a needle or catheter into the peritoneal cavity to extract fluid. The procedure serves diagnostic and therapeutic purposes:
Diagnostic: Fluid is analyzed to determine the cause of its accumulation, such as infections, cancer, or other conditions.
Therapeutic: It alleviates symptoms caused by fluid buildup, such as abdominal discomfort or difficulty breathing.
2. What are the indications and contraindications for abdominal paracentesis?
Indications: The procedure is performed in cases such as evaluating ascites due to liver cirrhosis or cancer, suspecting bacterial or tuberculous peritonitis, or relieving severe symptoms caused by fluid accumulation.
Contraindications: These include conditions requiring urgent surgical intervention, severe coagulopathy (INR > 2.0 or platelet count < 50,000), pregnancy, or extensive abdominal adhesions from previous surgeries.
3. How is abdominal paracentesis performed, and what are the potential complications?
The procedure involves identifying the insertion site (usually below the navel or on the sides), applying local anesthesia, and inserting a needle or catheter to extract the fluid.
Positioning: The patient is placed in a lying or semi-Fowler's position (30-45 degrees) to facilitate fluid collection.
Complications: Possible risks include bleeding or hematoma at the insertion site, infection, fluid leakage, or, rarely, intestinal perforation, hypovolemia, or circulatory dysfunction.
4. What causes reaccumulation of peritoneal fluid, and how is it managed?
Fluid reaccumulation may result from conditions such as liver cirrhosis with portal hypertension, cancer, heart failure, nephrotic syndrome, tuberculous peritonitis, or pancreatic disorders.
Management: Treating the underlying cause (e.g., diuretics for cirrhosis, chemotherapy for cancer), dietary modifications (reducing sodium and increasing protein), repeated paracentesis as needed, or advanced interventions like peritoneovenous shunting or liver transplantation in severe cases.
5. What are the health benefits of fasting outside Ramadan?
Fasting outside Ramadan, such as intermittent fasting, offers numerous health benefits, including:
Improved insulin sensitivity and lower blood sugar levels.
Enhanced fat metabolism and weight loss.
Stimulation of autophagy (cellular repair).
Boosting the immune system.
Improved cognitive function and memory.
6. What are the benefits of cold water therapy, and how does it promote health?
Cold water therapy, through cold showers or immersion, provides several benefits, such as:
Reducing inflammation.
Enhancing circulation.
Strengthening immune response.
Alleviating symptoms of anxiety and depression.
Cold water stimulates blood flow and releases endorphins, which improve mood.
7. What are the health benefits of honey, particularly Manuka honey?
Honey, especially Manuka honey, possesses unique therapeutic properties due to its natural sugars, enzymes, antioxidants, and bioactive compounds.
Accelerates wound healing.
Supports digestive health.
Boosts the immune system.
Keywords:
Abdominal paracentesis, diagnostic, therapeutic, peritoneal fluid, ascites, cirrhosis, liver disease, malignancy, peritonitis, procedure, complications, reaccumulation, fasting, cold water therapy, honey, Manuka honey, wound healing, inflammation, metabolic health, immune support.