malignancy carcinogens : autophagy fasting
Discover how oxidative stress, chemotherapy, and radiotherapy play a crucial role in preventing malignancy.
CANCER
Dr Hassan Al Warraqi
5/21/2024
malignancy carcinogens : autophagy fasting
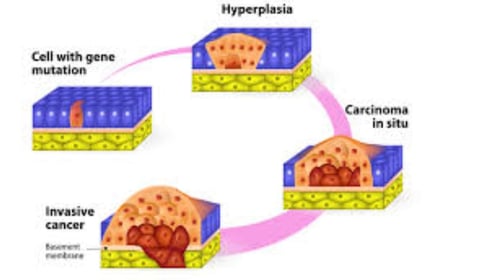
is a medical term used to describe a type of cell growth that has the potential to become cancerous.
Malignant cells are abnormal cells that divide uncontrollably and can invade nearby tissues
They can also spread to other parts of the body through the blood and lymphatic systems.
the presence of cancerous cells that have the ability to spread to other sites in the body (metastasize) or to invade nearby (locally) and destroy tissues
tend to have fast, uncontrolled growth and do not die normally due to changes in their genetic makeup
resistant to treatment and may return after all detectable traces of them have been removed or destroyed
They can spread to nearby tissues and to distant parts of the body
genome instability, often having between 10,000 and 100,000 mutations in their entire genomes
A biopsy is typically required to distinguish whether a tumor is malignant or benign
Key Characteristics of Malignancy:
Uncontrolled Cell Growth: Malignant cells proliferate without the normal regulatory mechanisms that control cell division and growth
Invasiveness: These cells can invade surrounding tissues, breaking through normal tissue barriers
Metastasis: Malignant cells can spread to distant parts of the body via the bloodstream or lymphatic system.
Genetic Mutations: Malignant cells often have mutations in their DNA that contribute to their aggressive behavior.
Resistance to Apoptosis: They resist programmed cell death, allowing them to survive longer than normal cells.
Types of Malignant tumor
Carcinoma: the most common type of malignancy, and it begins in the epithelial cells that line the surface of organs and tissues
Sarcoma: malignancy starts in the connective tissues of the body, such as bones, muscles, and nerves
Leukemia: This is a cancer of the blood and bone marrow
Lymphoma: This is a cancer of the lymphatic system
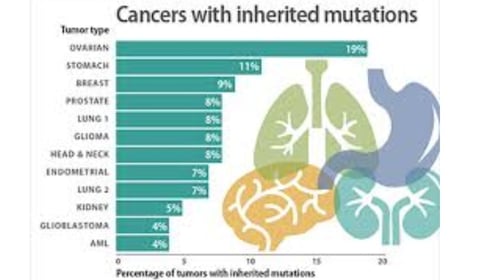
can be caused by a variety of factors, including genetics, exposure to carcinogens (such as tobacco smoke and ultraviolet radiation), and certain viruses
Early detection and treatment is essential for improving the chances of a successful outcome
While there's no guaranteed way to prevent
malignancy entirely
there are several lifestyle changes and precautions you can take to significantly reduce your risk
RA is slightly above that of the general population
secondary to an increased risk of lymphomas
Regular Screenings and Vaccinations
Screening Tests:include:
Mammograms for breast cancer
Pap tests and HPV tests for cervical cancer
Colonoscopy for colorectal cancer
Low-dose CT scans for lung cancer in high-risk individuals
Vaccinations:
HPV Vaccine: Protects against human papillomavirus, which can cause cervical and other cancers.
Hepatitis B Vaccine: Reduces the risk of liver cancer caused by hepatitis B virus.
Avoiding Carcinogens
Environmental and Occupational Hazards: Reduce exposure to known carcinogens such as asbestos, radon, and certain chemicals used in industries.
Radiation Exposure: such as X-rays and CT scans, and ensure proper shielding if exposed to radiation in the workplace.
Medical Interventions
Chemoprevention: The use of drugs or other substances to reduce the risk of developing cancer in high-risk individuals.
Genetic Counseling and Testing: For individuals with a family history of cancer, genetic counseling and testing can identify inherited cancer risk and lead to proactive measures such as increased surveillance or preventive surgeries.
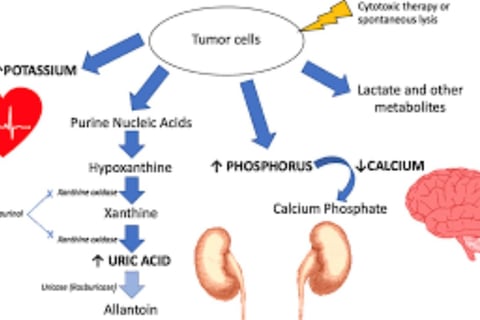
Prophylactic Measures: Patients at low, intermediate, or high risk of developing tumor lysis syndrome (TLS) should be identified early
TLS after the treatment of a malignancy with chemotherapy and/or radiotherapy, resulting from extreme tumor cell lysis with the release of intracellular contents
healthy life style
Maintain a healthy weight:Being overweight or obese is a risk factor for many malignancies
including breast, colon, and endometrial cancer
Eat a healthy diet:A diet rich in fruits
vegetables, and whole grains and low in processed meats, red meat, and sugary drinks can help reduce your risk of malignancy
Be physically active:Aim for at least 30 minutes of moderate-intensity exercise most days of the week
Regular physical activity can help you maintain a healthy weight and reduce your risk of many malignancies
Don't smoke:Smoking is a major risk factor for lung cancer, as well as many other malignancies
Limit alcohol consumption: Heavy alcohol consumption can increase your risk of several malignancies, including mouth, throat, esophagus, liver, and breast cancer
Protect yourself from the sun: Ultraviolet (UV) radiation from the sun can damage your skin and increase your risk of skin cancer
wear sunscreen whenever you are outdoors
Get vaccinated:Vaccinations can help protect you from certain viruses that can increase your risk of malignancy, such as hepatitis B and human papillomavirus (HPV)
Get regular cancer screenings: Early detection is key to successful malignancy treatment
Islamic Fasting
Detoxification: Periods of fasting can help detoxify the body by giving the digestive system a rest, which may reduce the buildup of potentially harmful substances
Cellular Repair and Autophagy: Fasting triggers autophagy, a process where cells remove damaged components and regenerate new ones, which can help eliminate precancerous cells
Weight Management: Fasting can help reduce body weight and fat, lowering the risk of obesity-related cancers
Insulin Sensitivity: improves insulin sensitivity and reduces blood sugar levels, decreasing the risk of cancer, particularly those linked to high insulin levels like breast and colon cancer
Inflammation Reduction: Fasting can decrease levels of inflammation, which is linked to cancer development
Intermittent Fasting
IF) involves cycling between periods of eating and fasting include
the 16/8 method (16 hours fasting, 8 hours eating) and
the 5:2 method (normal eating for 5 days, very low calorie intake for 2 days)
The potential anti-cancer benefits of IF
Improved Metabolic Health: IF can lead to improved metabolic markers, such as lower insulin levels and improved blood sugar control, reducing the risk of cancers associated with metabolic syndrome
Reduction in Oxidative Stress and Inflammation: reduce oxidative stress and inflammation
Hormonal Changes: Fasting can decrease levels of growth factors like insulin-like growth factor 1 (IGF-1), which is linked to cancer progression
Enhanced Autophagy: Similar to Islamic fasting, intermittent fasting enhances autophagy, helping to clear out damaged cells and prevent cancerous transformations
Weight Loss and Fat Reduction: promoting weight loss and reducing visceral fat, IF can lower the risk of obesity-related cancers
intermittent fasting can reduce tumor growth
Research has indicated that the caloric restriction from fasting can delay the onset of cancer and increase survival
Practical Considerations
Consistency: The benefits of fasting are often linked to consistency and long-term adherence
Individual Health: Fasting may not be suitable for everyone , pregnant or breastfeeding women, or individuals with a history of eating disorders
Nutritional Balance: During eating periods, it’s important to maintain a balanced diet rich in fruits, vegetables, lean proteins, and whole grains to support overall health and prevent nutrient deficiencies
keywords
Malignancy, carcinogens, Uncontrolled , autophagy , oxidative stress , chemotherapy , radiotherapy , surgical , prevention ,fasting , caloric restriction from, fasting, can delay the onset of cancer, and increase survival,
Cancerous Tumors, Carcinogens, and Autophagy: Mechanisms, Relationships, and Therapeutic Implications
1. Cancerous Tumors (Malignancy)
Definition:
Malignant tumors are abnormal cells that grow and divide uncontrollably, invading surrounding tissues and spreading to distant organs via blood or the lymphatic system (metastasis).
Key Features:
Uncontrolled Growth: Cancer cells evade normal cell death mechanisms due to genetic mutations.
Treatment Resistance: They often resist therapies and may recur even after apparent eradication.
Diagnosis: Requires a biopsy to confirm malignancy.
Types:
Carcinoma: Originates in epithelial tissues (e.g., breast, lung).
Sarcoma: Arises in connective tissues (e.g., bone, muscle).
Leukemia: Affects blood-forming tissues.
Lymphoma: Targets the lymphatic system.
Causes:
Genetic predisposition.
Exposure to carcinogens (e.g., tobacco smoke, UV radiation).
Viral infections (e.g., HPV).
2. Carcinogens
Definition:
Carcinogens are substances or environmental factors that trigger normal cells to become cancerous.
Examples:
Chemical: Pesticides, industrial plastics, asbestos.
Radiation: UV rays, nuclear radiation.
Biological: Viruses (e.g., HPV, hepatitis B).
Lifestyle: Tobacco smoke, alcohol.
Prevention:
Use sunscreen.
Vaccination (e.g., HPV vaccine).
Regular cancer screenings.
3. Autophagy
Definition:
Autophagy is a cellular recycling process where cells break down damaged components (e.g., proteins, organelles) for reuse.
Types:
Macroautophagy: Primary mechanism (often referred to as autophagy).
Microautophagy: Direct engulfment by lysosomes.
Chaperone-Mediated Autophagy (CMA): Selective protein degradation.
Mechanism:
Induction: Triggered by nutrient deprivation, oxidative stress, or mTOR inhibitors (e.g., rapamycin).
Phagophore Formation: A double membrane isolates cellular debris.
Maturation: Forms an autophagosome.
Fusion: Merges with lysosomes to create an autolysosome.
Degradation: Enzymes recycle components (e.g., amino acids).
Dual Role in Cancer:
Early Stages: Acts as a tumor suppressor by removing damaged cells.
Advanced Stages: Supports tumor survival under metabolic stress (e.g., nutrient deprivation).
4. Carcinogens, Autophagy, and Cancer
Carcinogens may activate or disrupt autophagy, influencing cancer progression.
Stress from carcinogens can trigger autophagy as a survival mechanism.
Dysregulated autophagy contributes to treatment resistance and tumor growth.
5. Autophagy as a Cancer Therapeutic Target
Strategies:
Inhibition: Blocking autophagy in advanced cancers (e.g., chloroquine).
Activation: Enhancing autophagy in early stages (e.g., rapamycin).
Intermittent Fasting (IF): Fasting activates autophagy, potentially delaying cancer onset and improving treatment outcomes.
Clinical Evidence:
Preclinical studies show fasting reduces tumor growth by 35% in mice.
Human trials suggest fasting during chemotherapy reduces side effects.
6. Autophagy-Related Genes and Cancer
Beclin1: A tumor suppressor gene often mutated in cancers.
ATG5/ATG7: Critical for autophagy; mutations promote tumorigenesis.
PI3K/Akt/mTOR Pathway: Dysregulation drives cancer progression.
7. Voluntary Fasting, Autophagy, and Cancer
Mechanisms:
Autophagy Activation: Fasting triggers AMPK and inhibits mTOR, promoting cellular cleanup.
Metabolic Disruption: Starves glucose-dependent cancer cells.
Immune Enhancement: Regenerates immune cells and reduces inflammation.
Benefits:
Reduces obesity, insulin resistance, and chronic inflammation (cancer risk factors).
Enhances chemotherapy efficacy via differential stress resistance.
Precautions:
Contraindicated for underweight patients or those with malnutrition.
Requires medical supervision during cancer treatment.
8. Recommendations
Research: Investigate autophagy’s role in specific cancers and stages.
Therapeutic Development: Test autophagy modulators (e.g., chloroquine, rapamycin) in clinical trials.
Public Awareness: Promote carcinogen avoidance and healthy lifestyles.
Fasting Protocols: Explore intermittent fasting as an adjuvant therapy.
Conclusion
The interplay between malignancy, carcinogens, and autophagy is complex.
While autophagy can suppress early tumors, it may fuel advanced cancers.
Understanding these dynamics is critical for developing therapies targeting autophagy.
Voluntary fasting shows promise in cancer prevention and treatment but requires further clinical validation.
SEO Keywords
Cancer prevention, autophagy mechanisms, carcinogens, tumor suppression, intermittent fasting, chemotherapy efficacy, mTOR pathway, Beclin1 gene, tumor recurrence.
FAQs on Cancerous Tumors, Carcinogens, and Autophagy
What are cancerous tumors, and how do they develop?
Cancerous tumors arise from abnormal cells that grow and divide uncontrollably, bypassing the body’s natural regulatory mechanisms.
These invasive cells can:
Invade nearby tissues and disrupt normal organ function.
Spread to distant organs via the bloodstream or lymphatic system, forming secondary tumors (metastases).
Resist programmed cell death (apoptosis) and accumulate genetic mutations due to genomic instability.
Key Features:
Rapid, unregulated growth.
Resistance to treatment and potential recurrence.
Genetic mutations driving tumor evolution.
What are carcinogens, and what are their main types?
Carcinogens are substances or environmental factors that trigger normal cells to become cancerous.
Major types include:
Chemical Carcinogens:
Tobacco smoke (contains over 70 carcinogens).
Industrial chemicals (e.g., asbestos, benzene).
Pesticides and plastics (e.g., bisphenol A).
Physical Carcinogens:
Ultraviolet (UV) radiation (sunlight, tanning beds).
Ionizing radiation (X-rays, nuclear radiation).
Biological Carcinogens:
Viruses (e.g., HPV, hepatitis B/C).
Bacteria (e.g., H. pylori linked to stomach cancer).
Prevention Tip: Minimize exposure through protective measures like sunscreen, workplace safety protocols, and vaccinations (e.g., HPV vaccine).
What is autophagy, and what is its normal role in cells?
Autophagy is a cellular recycling process where cells degrade and reuse damaged components (e.g., proteins, organelles). Its functions include:
Cellular Housekeeping: Removing dysfunctional components to maintain cell health.
Energy Production: Recycling nutrients during starvation or stress.
Pathogen Clearance: Eliminating intracellular pathogens.
Quality Control: Preventing protein aggregates linked to diseases like Alzheimer’s.
Key Insight: Autophagy is essential for cellular homeostasis and longevity.
How do carcinogens affect autophagy?
Carcinogens can disrupt or hijack autophagy in complex ways:
Activation: Some carcinogens (e.g., UV radiation) trigger autophagy as a survival mechanism, helping cells tolerate DNA damage.
Suppression: Chronic exposure to toxins (e.g., alcohol) may impair autophagy, leading to toxin buildup and cancer progression.
Dual Effects: The impact depends on carcinogen type, exposure duration, and cell context.
Example: Tobacco smoke suppresses autophagy in lung cells, promoting tumor growth.
What is autophagy’s dual role in cancer development?
Autophagy acts as a double-edged sword in cancer:
Tumor Suppression (Early Stages):
Clears damaged proteins/organelles to prevent mutations.
Triggers apoptosis in pre-cancerous cells.
Tumor Promotion (Advanced Stages):
Fuels cancer cell survival under stress (e.g., nutrient deprivation in tumors).
Enhances resistance to chemotherapy and radiation.
Clinical Relevance: Targeting autophagy requires stage-specific strategies.
What molecular mechanisms regulate autophagy?
Autophagy is governed by key pathways and proteins:
mTOR Kinase: Inhibits autophagy when nutrients are abundant.
AMPK: Activates autophagy during energy stress.
ULK1 Complex: Initiates autophagosome formation.
ATG Proteins: Mediate autophagosome expansion and cargo recognition (e.g., LC3, p62/SQSTM1).
Lysosomal Fusion: Autophagosomes merge with lysosomes for component breakdown.
Drug Targets: Rapamycin (mTOR inhibitor) and chloroquine (lysosomal inhibitor) are used to modulate autophagy.
How can autophagy be targeted in cancer therapy?
Therapeutic Strategies:
Autophagy Inhibition:
Drugs: Chloroquine/hydroxychloroquine block lysosomal degradation.
Use Case: Enhances chemotherapy efficacy in resistant tumors.
Autophagy Activation:
Drugs: Rapamycin analogs (e.g., everolimus) induce autophagy.
Use Case: Clears pre-cancerous cells in early-stage tumors.
Intermittent Fasting (IF):
Triggers autophagy, reduces inflammation, and starves cancer cells.
Clinical Trials: IF combined with chemo shows reduced side effects in breast cancer patients.
What are key preventive strategies to reduce cancer risk?
Evidence-Based Prevention:
Avoid Carcinogens: Quit smoking, limit alcohol, and reduce UV exposure.
Vaccinations: HPV and hepatitis B vaccines lower viral-linked cancer risks.
Screening: Regular mammograms, colonoscopies, and Pap smears for early detection.
Healthy Lifestyle:
Diet: Antioxidant-rich foods (berries, leafy greens).
Exercise: 150+ minutes/week of moderate activity.
Weight Management: Reduce obesity-linked cancers (e.g., breast, colon).
Intermittent Fasting:
May lower cancer risk by enhancing autophagy and metabolic health.
SEO Keywords:
Cancerous Tumors, Carcinogens, Autophagy Mechanism, Tumor Suppression, Metastasis, Chemotherapy Resistance, Intermittent Fasting, mTOR Pathway, Cancer Prevention, Chloroquine, Rapamycin.
Conclusion:
Understanding the interplay between carcinogens, autophagy, and tumor biology is critical for advancing cancer therapies.
While autophagy modulation holds promise, personalized approaches are essential. Always consult healthcare providers before adopting fasting or experimental treatments.
Explore Further:
National Cancer Institute: www.cancer.gov
World Health Organization (WHO): Cancer Prevention Guidelines.